10 Dec 2025
- 15 Comments
Anticholinergic Burden Calculator
Enter your medications to calculate your cumulative anticholinergic burden score. The ACB Scale rates drugs from 0 to 3 based on their anticholinergic effects.
Every year, thousands of older adults in the UK and beyond are admitted to hospital for confusion, falls, or memory problems-often without anyone realizing the real cause is something they’re taking every night before bed. It’s not dementia. It’s not aging. It’s cumulative anticholinergic burden.
What Exactly Is Anticholinergic Burden?
Your body uses a chemical called acetylcholine to help you think, move, digest food, and even control your bladder. Anticholinergic medications block this chemical. That’s fine if you’re taking one drug for a short time, like an antihistamine for a bad allergy. But when you take several of these drugs over months or years, their effects add up. That’s the burden.First-generation antihistamines like diphenhydramine (Benadryl) and chlorpheniramine are strong blockers. They’re in sleep aids, cold meds, and allergy pills you can buy without a prescription. Many people don’t think twice about popping one at night. But if you’re also taking amitriptyline for nerve pain, oxybutynin for an overactive bladder, or even a low-dose antipsychotic for sleep, you’re stacking up the anticholinergic effects.
The ACB Scale-developed in 2008 and now used in clinics across the UK and US-rates drugs on a scale from 0 to 3. A score of 0 means no anticholinergic effect. A score of 3 means strong. Diphenhydramine? Score 3. Chlorpheniramine? Score 3. Amitriptyline? Score 3. Oxybutynin? Score 3. Loratadine (Claritin)? Score 0. Cetirizine (Zyrtec)? Score 1.
When your total score hits 3 or higher, your risk of cognitive decline, falls, and hospitalization jumps. A 2015 study in JAMA Internal Medicine followed over 3,400 people for seven years. Those who took strong anticholinergics daily for more than three years had a 54% higher risk of dementia. Antihistamines made up nearly a third of those strong drugs.
Why Antihistamines Are the Silent Culprit
Most people think of antihistamines as harmless allergy pills. But first-generation ones-diphenhydramine, promethazine, hydroxyzine-are designed to cross the blood-brain barrier. That’s why they make you drowsy. That same property makes them dangerous over time.Here’s the problem: 70% of strong anticholinergic drugs are available over the counter. No prescription needed. No warning label that says, “This may cause memory loss.” A 2022 survey on AgingCare.com found that 68% of caregivers said their doctor never mentioned the cognitive risks of long-term antihistamine use-even when the patient was over 70 and taking it nightly for sleep.
One Reddit user described how their 78-year-old mother was diagnosed with early dementia. She was on diphenhydramine every night and amitriptyline for chronic pain. Total ACB score: 6. After stopping both, her memory improved within weeks. Her doctor hadn’t connected the dots.
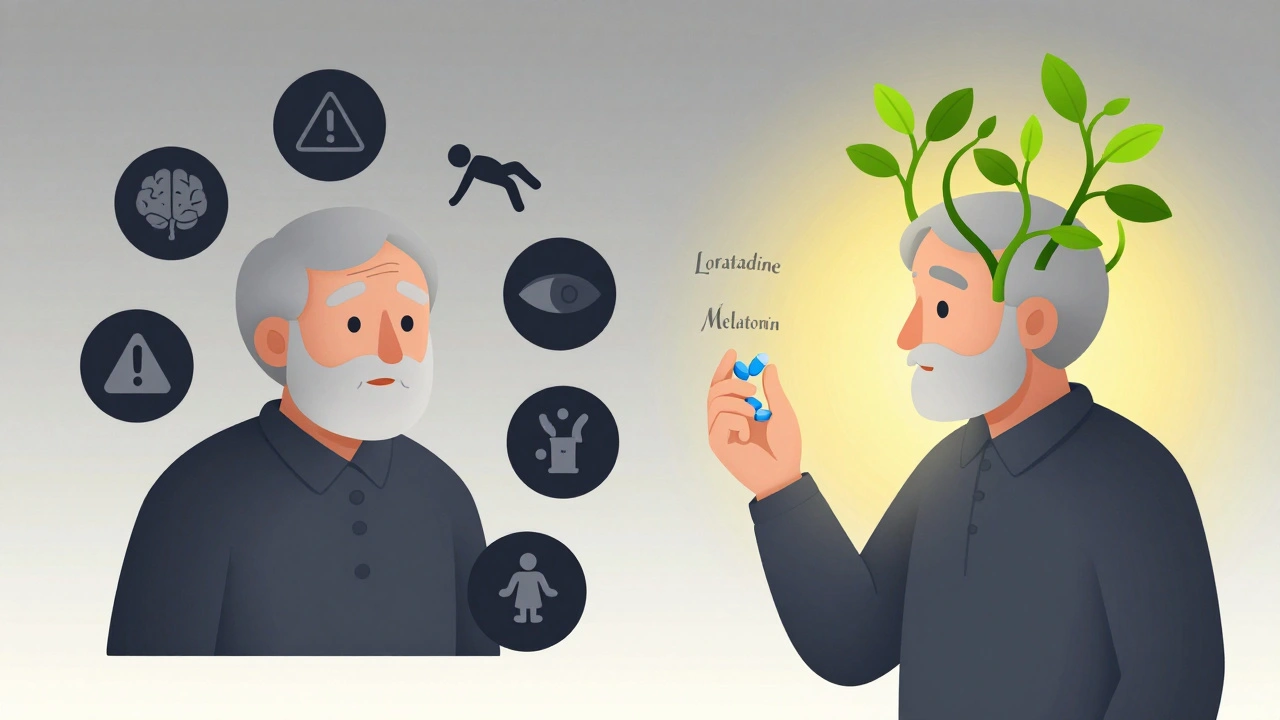
Second-generation antihistamines like loratadine, fexofenadine, and cetirizine don’t cross the brain barrier as easily. They’re just as good for allergies, with almost no anticholinergic effect. Yet, many older adults still reach for the old-school brands because they’re cheaper or they’ve used them for decades.
What Other Medications Make It Worse?
It’s not just antihistamines. It’s the combo. Here’s what commonly piles on:- Tricyclic antidepressants (amitriptyline, nortriptyline): Used for pain, depression, migraines. ACB score 3.
- Bladder meds (oxybutynin, tolterodine): For overactive bladder. ACB score 3.
- Parkinson’s drugs (benztropine, trihexyphenidyl): ACB score 2-3.
- Sleep aids (doxepin, promethazine): Even low doses add up. ACB score 2-3.
- Some heart and blood pressure meds (like certain diuretics): Mild effect, but still contribute.
Take a 72-year-old woman on amitriptyline (3), oxybutynin (3), and diphenhydramine (3). That’s a score of 9. She’s not just at risk-she’s in the danger zone. Studies show people with scores above 3 are 33% more likely to be hospitalized in a year. That’s not a small number.
The American Geriatrics Society’s Beers Criteria, updated in 2023, now says bluntly: “Avoid chronic use of first-generation antihistamines in older adults.” That’s not a suggestion. It’s a warning based on solid evidence.
What Symptoms Should You Watch For?
The signs aren’t always obvious. People think memory lapses are “just getting older.” But here’s what really happens:- Sudden confusion or trouble finding words
- Forgetfulness that doesn’t match their usual pattern
- Falls or dizziness, especially in the morning
- Constipation, dry mouth, blurred vision
- Urinary retention or difficulty starting to pee
- Increased agitation or hallucinations
These aren’t normal aging signs. They’re red flags. A 2021 patient guide from Hull University Teaching Hospitals found that 15-20% of older adults on multiple anticholinergics experience confusion. And in many cases, these symptoms reverse when the drugs are stopped.
One case study from NPS MedicineWise followed a 72-year-old man with an ACB score of 5. He was falling regularly, forgetting appointments, and struggling to follow conversations. After switching from diphenhydramine to loratadine and replacing amitriptyline with a non-anticholinergic pain option, his falls dropped by 75% in six months. His memory returned.
How to Reduce Your Burden
You don’t have to live with this risk. Here’s how to take control:- Make a full list of everything you take-prescription, over-the-counter, supplements, herbal remedies. Include dosages and how often.
- Check the ACB score for each. Use the free ACB Scale tool from the IU Center for Aging Research (searchable online). Diphenhydramine? 3. Chlorpheniramine? 3. Loratadine? 0.
- Ask your pharmacist or GP: “Could any of these be adding up to cause memory or balance problems?” Don’t be afraid to ask for alternatives.
- Switch to safer options. For allergies: use loratadine, fexofenadine, or cetirizine. For sleep: try melatonin, cognitive behavioural therapy for insomnia (CBT-I), or improved sleep hygiene. For bladder issues: consider pelvic floor exercises or mirabegron instead of oxybutynin.
- Don’t stop cold turkey. Some meds need to be tapered slowly. Work with your doctor to create a safe plan.
The NHS England 2022 Medicines Optimisation Strategy estimates that cutting anticholinergic burden could save £217 million a year in hospital admissions alone. That’s not just money-it’s independence, dignity, and quality of life.

What’s Changing in 2025?
Things are shifting. More GPs are being trained to check for anticholinergic burden. The NHS is rolling out automated alerts in electronic health records that flag patients with ACB scores above 3. The IU Center for Aging Research is leading a £2.8 million project to embed these alerts across UK primary care by 2026.Meanwhile, second-generation antihistamines now make up 85% of the allergy market in the UK. But among older adults, nearly half still use the old ones. Why? Familiarity. Cost. Lack of awareness.
It’s time to change that. If you’re over 50 and taking any antihistamine regularly-even just a few times a week-it’s worth asking: Is this helping me, or is it slowly stealing my memory?
Can antihistamines really cause dementia?
Yes, long-term use of first-generation antihistamines like diphenhydramine is linked to a higher risk of dementia, especially when combined with other anticholinergic drugs. A major 2015 study found people who took strong anticholinergics daily for over three years had a 54% higher risk. It’s not guaranteed, but the evidence is strong enough that doctors now advise avoiding them in older adults.
Is Zyrtec or Claritin safer than Benadryl?
Yes. Zyrtec (cetirizine) and Claritin (loratadine) are second-generation antihistamines with minimal anticholinergic effects. Their ACB score is 0-1, compared to Benadryl’s score of 3. They’re just as effective for allergies without the brain fog, dry mouth, or memory risks. Switching is safe and recommended for anyone over 50.
I’ve been taking diphenhydramine for sleep for years. Should I stop?
If you’re over 50 and taking it regularly, yes-talk to your doctor about stopping. It’s not an emergency, but it’s not harmless either. Many people experience improved memory and balance within weeks of stopping. Try melatonin, sleep hygiene changes, or CBT-I instead. Never quit cold turkey if you’ve been using it daily for months-your doctor can help you taper safely.
Can I check my own anticholinergic burden?
Yes. The ACB Scale is free and easy to use. List every medication you take-prescription and over-the-counter-and look up each one on the ACB Scale chart. Add up the scores. If you’re at 3 or higher, you’re in the risk zone. Bring this list to your GP or pharmacist. They can help you find safer alternatives.
Are there any side effects from stopping antihistamines?
If you’ve been using diphenhydramine nightly for sleep, you might have trouble falling asleep at first. That’s normal. It’s your body adjusting. Don’t go back to it. Use melatonin, a warm drink, or a quiet routine instead. For allergies, switching to loratadine or cetirizine will control symptoms without the drowsiness. Withdrawal from anticholinergics doesn’t cause physical dependence-it just means your brain is no longer being chemically slowed down.
What to Do Next
Start today. Take out your pill bottle or medicine cabinet. Write down every medication you take, including what you buy at the pharmacy without a prescription. Look up each one on the ACB Scale. If your total is 3 or more, make an appointment with your GP or pharmacist. Bring the list. Ask: “Could any of these be affecting my memory or balance?”Most people don’t realize their daily habits are quietly harming their brain. But once they know, they can change. And that change can mean more years of clear thinking, fewer falls, and more independence.

Paul Dixon
December 12, 2025I had no idea Benadryl was this dangerous long-term. My grandma took it every night for years and we thought she was just getting forgetful. Turns out it was the meds. Switched her to melatonin and her memory cleared up in weeks. So simple, yet no one ever told us.
Jim Irish
December 13, 2025This is critical information. The cumulative effect of anticholinergics is underrecognized in primary care. Elderly patients are often prescribed multiple agents without consideration of pharmacodynamic synergy. A systematic review of this burden is long overdue.
Mia Kingsley
December 14, 2025ok but like... isnt all this just fearmongering? i mean my auntie takes benadryl and she still dances at weddings. also i think zyrtec is just a big pharma scam to make you buy more stuff. also i read on a blog that dementia is just a myth created by the government to control old people. lol
Aidan Stacey
December 15, 2025Y’ALL. I just pulled my mom’s medicine cabinet. She’s on amitriptyline, oxybutynin, AND diphenhydramine. That’s a 9. A NINE. I almost cried. We’re going to the pharmacist tomorrow. I’m printing out the ACB scale and handing it to her doctor like it’s a damn manifesto. This isn’t just health-it’s dignity.
matthew dendle
December 15, 2025so you mean to tell me that the thing that lets me sleep through my kids crying is actually killing my brain? wow. thanks for the guilt trip. next youll tell me coffee gives you cancer
Monica Evan
December 16, 2025My 74-year-old dad was on diphenhydramine for sleep and amitriptyline for sciatica. Total ACB score: 6. He was walking like he was drunk, forgetting his own birthday. We switched him to gabapentin and loratadine. He’s been hiking again. No more falls. No more confusion. Just... him. If you’re over 50 and using OTC sleep aids, please check your meds. It’s not hype-it’s science.
Courtney Blake
December 16, 2025Of course the NHS wants you to stop using Benadryl. They’re trying to cut costs. My grandma lived to 92 on diphenhydramine. Who are you to tell older people what to take? This is America, not Sweden. Also, I’m not paying for fancy allergy pills just because some study says so.
Lisa Stringfellow
December 18, 2025So you’re saying I can’t have a nice night’s sleep anymore? What’s next? No more chocolate? No more warm milk? You people are obsessed with fear. My brain is fine. I’m not some lab rat for your clinical guidelines.
Kristi Pope
December 20, 2025This is the kind of post that makes me feel hopeful. So many of us are just trying to get through the day, and no one ever tells us these hidden dangers. I just checked my dad’s meds-three 3s. We’re going to make a plan together. Thank you for sharing this. You’ve given us a gift.
Aman deep
December 21, 2025Wow. I’m from India and we use diphenhydramine like candy here. No one talks about brain risks. My uncle takes it for allergies and sleep. I’m sending him this right now. Maybe we can save his mind before it’s too late. Thank you for writing this.
Eddie Bennett
December 23, 2025My therapist says my anxiety makes me hyperfixate on meds and side effects. But honestly? This scared me enough to actually look at my own bottle. I’ve been taking Benadryl for 12 years. I didn’t realize it was making me foggy during Zoom calls. I’m switching to Claritin tomorrow. No drama. Just… better.
Sylvia Frenzel
December 24, 2025Why are we always being told what to take? Nobody asked me if I wanted to live longer. I want to sleep. I don’t care if I forget my keys. Let me have my peace.
Vivian Amadi
December 26, 2025So you’re saying my 80-year-old neighbor who takes 5 different meds and sleeps like a rock is just dumb? She’s fine. You’re just trying to make people paranoid so you can sell your ‘safe’ alternatives. Wake up.
Jimmy Kärnfeldt
December 26, 2025It’s funny how we treat our bodies like machines we can just keep running with duct tape and Benadryl. We don’t think twice about adding another layer of chemical bandaids. But the brain? It doesn’t scream. It just… dims. Slowly. Until one day, you don’t recognize your own voice in the mirror.
Ariel Nichole
December 27, 2025My mom switched from Benadryl to Zyrtec last year. She says she feels more alert and doesn’t get that dry mouth anymore. I didn’t even know it was a thing. Thanks for making me look closer. I’m checking my own meds now.