ACE inhibitor vs ARB: What’s the Real Difference?
When working with ACE inhibitor vs ARB, the side‑by‑side comparison of two major blood‑pressure drug families that act on the renin‑angiotensin system. Also known as ACEI vs ARB, it helps doctors and patients decide which pathway fits a given health profile.
An ACE inhibitor, a medication that blocks the conversion of angiotensin I into the powerful vasoconstrictor angiotensin II (often called ACEI) reduces blood‑vessel tightening and lowers blood pressure. In contrast, an Angiotensin II receptor blocker, a drug that stops angiotensin II from binding to its receptor, preventing the vessel‑narrowing effect, is commonly referred to as ARB. Both target the same hormonal cascade but intervene at different steps – a classic example of the semantic triple: ACE inhibitor vs ARB encompasses ACE inhibitor and ACE inhibitor vs ARB encompasses ARB. The primary condition they treat is Hypertension, long‑term high arterial pressure that raises the risk of heart attack, stroke, and kidney damage. They’re also staples in managing Heart failure, a state where the heart can’t pump enough blood to meet the body’s needs, because lowering pressure eases the heart’s workload.
Key factors to compare
First, look at the mechanism. ACE inhibitors stop the enzyme that creates angiotensin II, so the hormone never forms. ARBs let angiotensin II form but block its receptor, so the hormone can’t act. This tiny difference changes the side‑effect profile. Because ACE inhibitors also raise bradykinin levels, they can cause a dry cough in up to 20 % of users. ARBs rarely cause cough, making them a go‑to when patients can’t tolerate the ACE‑related tickle.
Second, consider efficacy. Large trials show both classes lower systolic pressure by about 10–12 mm Hg on average. For most people, the drop is comparable, but ARBs might have a slight edge in reducing protein loss in the kidneys of diabetic patients. That’s why many nephrologists start with an ACE inhibitor for early kidney protection and switch to an ARB if cough becomes a problem.
Third, think about safety in special groups. Pregnant women must avoid both classes because interfering with angiotensin signaling can harm fetal kidney development. However, ACE inhibitors are especially risky in the second and third trimesters, while ARBs share the same warning. In patients with high potassium levels, both drugs can raise potassium further, so regular lab checks are a must.
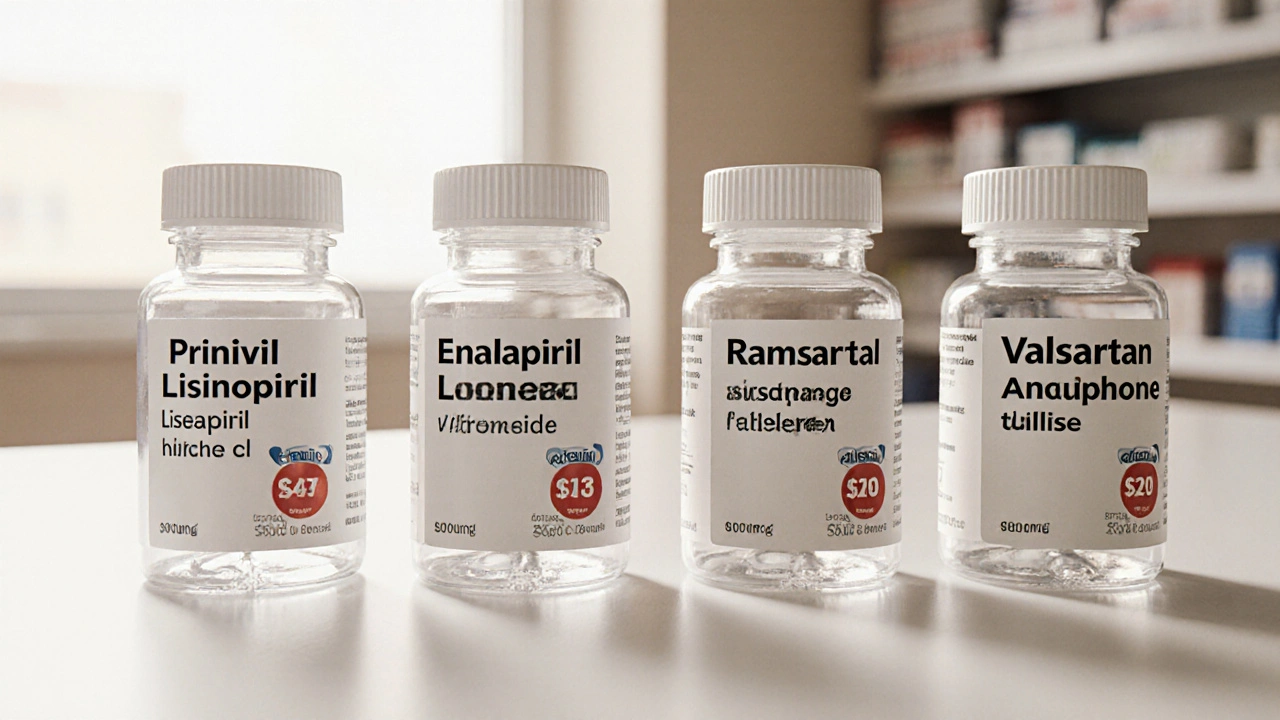
Cost is another practical piece. Most ACE inhibitors—like lisinopril, enalapril, and ramipril—are available as cheap generics. ARBs were under patent for years, but now drugs like losartan, valsartan, and irbesartan are also generic, narrowing the price gap. Insurance formularies often list one class as the preferred option, so checking your plan can save a few dollars each month.
Patient preference plays a big role too. If a person values once‑daily dosing, many ARBs (e.g., losartan) offer that convenience, while some ACE inhibitors need twice‑daily dosing. On the other hand, patients who have a history of angio‑edema should avoid both classes, but ARBs are sometimes tried after a severe ACE‑induced episode because they don’t affect the same pathway that triggered the swelling.
Finally, look at drug interactions. ACE inhibitors can boost the effect of potassium‑sparing diuretics and certain NSAIDs, potentially raising blood pressure or potassium too much. ARBs share many of those interactions but tend to have a slightly lower risk of worsening kidney function when combined with NSAIDs, though the difference is modest.
Putting it all together, the decision between an ACE inhibitor and an ARB often boils down to tolerance (cough vs none), specific organ protection needs (kidney vs heart), cost considerations, and individual lifestyle factors. Both classes have decades of safety data, so you’re unlikely to pick a “wrong” one as long as you monitor labs and watch for side effects.
Below you’ll find a curated list of articles that dive deeper into each point—mechanisms, side‑effect management, cost comparisons, and real‑world switching strategies. Use them to fine‑tune the choice that best fits your health goals, whether you’re just starting treatment for high blood pressure or looking to switch after an unwanted cough.
Prinivil (Lisinopril) vs Alternatives: Best Blood Pressure Choice
A detailed side‑by‑side comparison of Prinivil (Lisinopril) with top ACE inhibitors, ARBs, and other blood‑pressure drugs, covering cost, side effects, and when each is best to use.