Blood Pressure Pills – A Practical Overview
When dealing with blood pressure pills, medications prescribed to lower high arterial pressure and protect the heart and vessels. Also known as antihypertensives, they are a cornerstone in managing hypertension and preventing strokes, heart attacks, and kidney damage. blood pressure pills come in several classes, each working in a different way to calm the circulatory system.
Major Classes of Antihypertensive Medications
One of the most common groups is ACE inhibitors, drugs that block the enzyme converting angiotensin I to angiotensin II, a potent vessel‑tightening hormone. They often help people with diabetes or kidney disease because they also reduce protein loss in urine. Another big player is beta blockers, agents that slow heart rate and lower the force of contraction, easing the workload on the heart. For patients who need a smoother blood‑flow control, calcium channel blockers, medications that relax the smooth muscle in arterial walls, are a solid choice. Lastly, diuretics, often called water pills, help the kidneys remove excess salt and fluid, decreasing blood volume, serve as a first‑line option for many.
These four entities interact in predictable ways: ACE inhibitors lower angiotensin II, beta blockers curb heart rhythm, calcium channel blockers widen vessels, and diuretics reduce overall fluid load. Choosing the right mix often depends on age, kidney function, and other meds a patient is already taking. For example, a senior with a history of gout might avoid thiazide diuretics because they can raise uric acid levels, while a young adult with migraine may benefit from a calcium channel blocker that also helps prevent headaches.
Beyond the drug classes, two other concepts shape how you use blood pressure pills: drug interactions and side‑effect profiles. Many antihypertensives can amplify the effects of over‑the‑counter pain relievers, especially NSAIDs, which can blunt the blood‑pressure‑lowering action. Likewise, combining ACE inhibitors with potassium‑rich supplements may raise potassium too high, risking heart rhythm problems. Side effects vary: ACE inhibitors often cause a dry cough, beta blockers can cause fatigue or cold hands, calcium channel blockers may lead to swelling in the ankles, and diuretics sometimes cause low potassium. Knowing these nuances helps you and your doctor pick a regimen you can stick with.
Monitoring is the glue that holds the whole process together. Home blood‑pressure cuffs, regular clinic visits, and occasional blood tests for electrolytes keep you from drifting into unsafe zones. When a new pill is added, you’ll likely see a short period where the dose is tweaked—this is normal as the body finds a new equilibrium. If you notice dizziness, sudden swelling, or persistent cough, it’s a signal to review the medication plan.
Below you’ll find a curated set of articles that dive deeper into specific comparisons, buying guides, and safety tips for antihypertensive drugs. Whether you’re comparing ACE inhibitors with ARBs, looking for cheap generic options, or learning how to manage side effects, the collection gives you actionable information to make informed choices about your blood pressure pills.
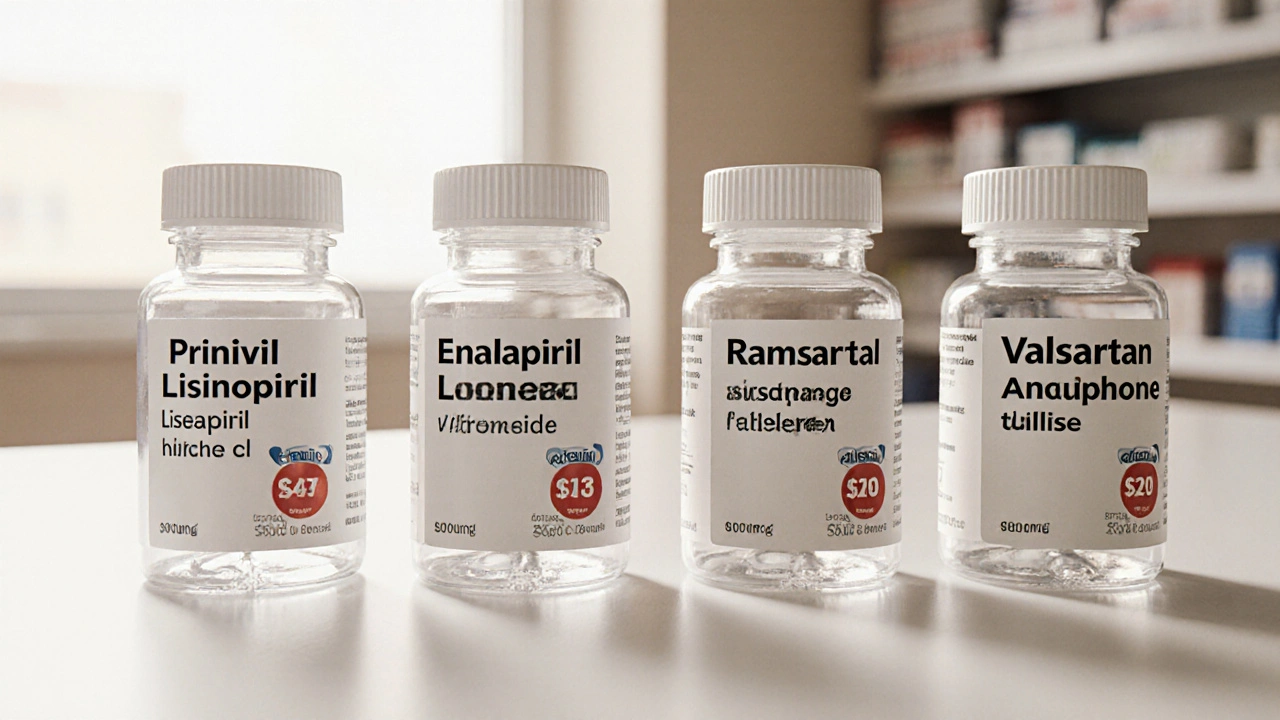
Prinivil (Lisinopril) vs Alternatives: Best Blood Pressure Choice
A detailed side‑by‑side comparison of Prinivil (Lisinopril) with top ACE inhibitors, ARBs, and other blood‑pressure drugs, covering cost, side effects, and when each is best to use.