8 Dec 2025
- 10 Comments
Asthma and COPD aren’t the same - even though they both make it hard to breathe
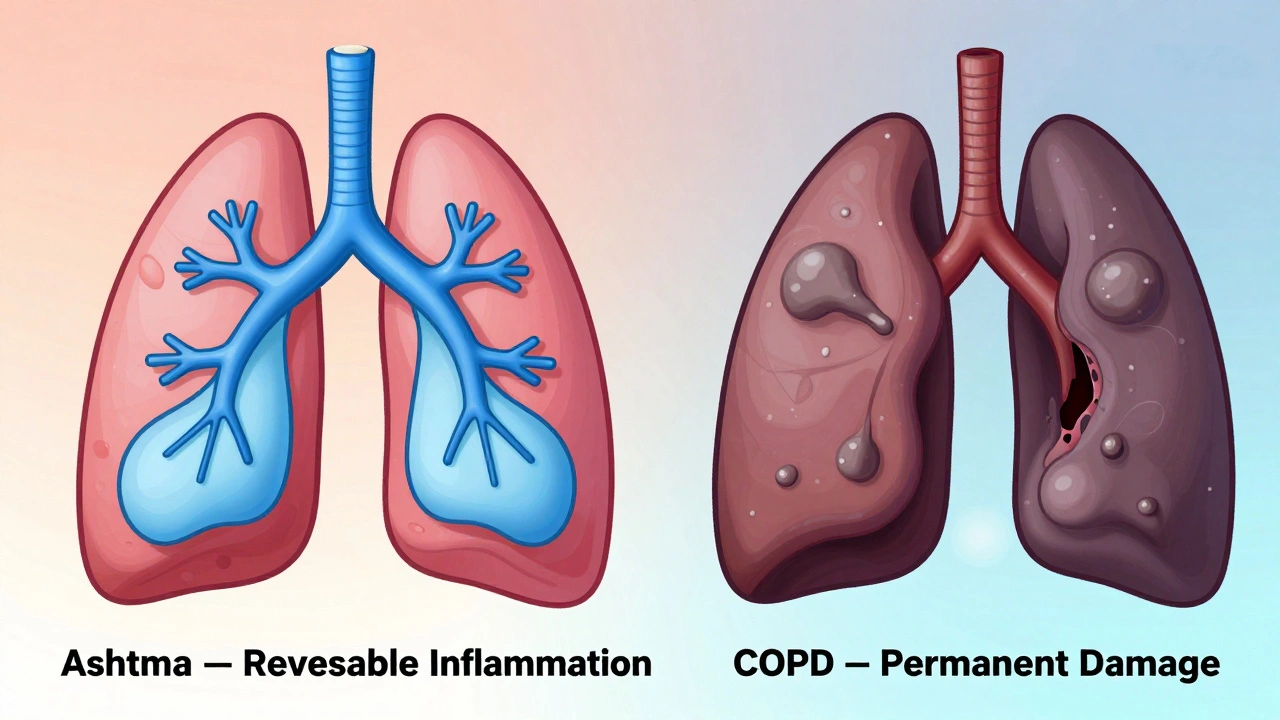
If you’re wheezing or struggling to catch your breath, it’s easy to assume it’s just asthma. But if you’re over 40 and have smoked for years, it might be something else: COPD. These two conditions look similar on the surface - coughing, shortness of breath, chest tightness - but they’re fundamentally different in how they develop, how they progress, and how they’re treated. Mixing them up can lead to the wrong meds, missed flare-ups, or even life-threatening delays in care.
Here’s what actually sets them apart - not just in theory, but in real life.
When do symptoms show up? Timing matters
Asthma often starts in childhood. About half of all cases are diagnosed before age 10. If you had frequent coughing or wheezing as a kid - especially after playing outside, during cold weather, or at night - you likely had asthma. Many people grow out of it. Others carry it into adulthood, but even then, symptoms usually come and go. You might feel fine for weeks, then get hit with a flare-up after a pollen storm or a cold.
COPD doesn’t work that way. It rarely shows up before age 40. Most people are diagnosed after 45, and nearly all cases are linked to long-term smoking. Unlike asthma, COPD symptoms don’t disappear between episodes. You won’t wake up one day and feel completely normal. Instead, you’ll notice a slow, steady decline: your cough gets worse, your breathlessness creeps in during simple tasks like walking to the mailbox, and you’re always clearing phlegm.
What does your cough sound like?
Not all coughs are created equal.
Asthma coughs are usually dry. You might feel a tickle in your throat or a tightness in your chest, but you don’t bring up much mucus. About 73% of asthma patients report a dry cough, especially at night or early morning.
COPD coughs are different. They’re wet. Constant. Productive. Around 87% of people with COPD cough up phlegm every day - often thick and yellow or green. This isn’t just a nuisance; it’s a sign of chronic bronchitis, one of the two main types of COPD. If you’ve been smoking for 20+ years and you’ve had a daily cough for months or years, that’s not “just a smoker’s cough.” It’s your lungs telling you something’s wrong.
Can you breathe normally between episodes?
This is one of the clearest differences.
Asthma patients often live symptom-free for long stretches. A 2022 study found that 68% of asthma patients have long periods with no symptoms at all. They can run, swim, travel, and sleep through the night - until a trigger hits. Then, their airways tighten suddenly. But with the right meds, they bounce back quickly.
COPD patients don’t get those breaks. Only 12% report any real period of symptom relief. Even on “good days,” their lungs are working harder than normal. You might not be wheezing, but climbing stairs leaves you winded. Carrying groceries feels like a workout. This isn’t aging - it’s lung damage that doesn’t heal.
How do doctors tell them apart?
It’s not just about symptoms. Doctors use tests to see what’s really going on inside your lungs.
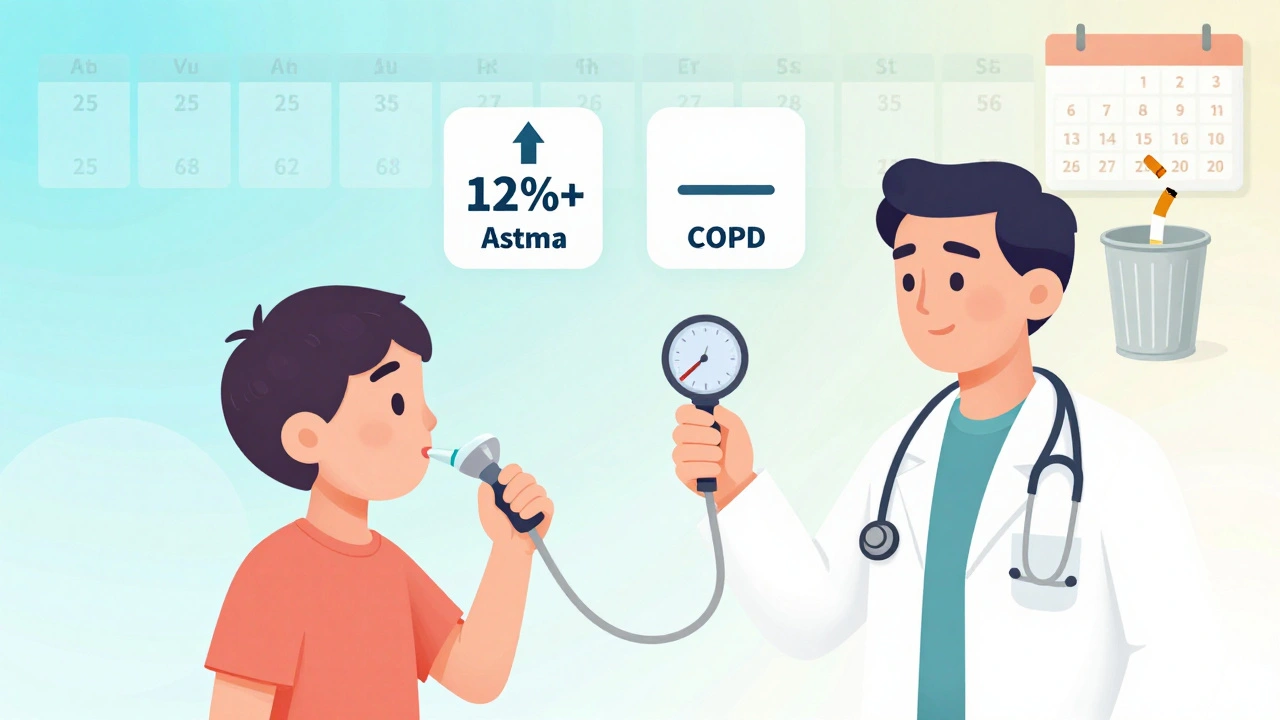
One key test is spirometry. You blow hard into a tube, and they measure how much air you can push out in one second (FEV1). Then you get a bronchodilator - a quick puff of albuterol - and you blow again.
If your FEV1 improves by 12% or more, it’s likely asthma. About 95% of asthma patients show this kind of reversibility. Their airways are inflamed and constricted, but they can open up again.
If your FEV1 barely changes - less than 12% improvement - it’s likely COPD. The damage is structural. The air sacs are destroyed (emphysema), or the airways are scarred and clogged (chronic bronchitis). Medications help you breathe easier, but they can’t reverse the damage.
Another tool is FeNO testing - measuring nitric oxide in your breath. High levels (above 50 ppb) point to eosinophilic inflammation, which is classic asthma. Low levels (below 25 ppb) suggest COPD. Blood tests for eosinophils (a type of white blood cell) help too: counts above 300 cells/μL lean toward asthma or overlap syndrome. Below 100? More likely pure COPD.
What treatments work for each?
Treatment plans are not interchangeable.
Asthma treatment starts with quick-relief inhalers - albuterol - for sudden attacks. If you’re having symptoms more than twice a week, you’ll likely move to daily inhaled corticosteroids (ICS) to calm the inflammation. For severe asthma with allergies, biologic drugs like omalizumab or mepolizumab target specific immune cells. These aren’t just inhalers - they’re precision tools. About 89% of asthma patients get good control with the right plan.
COPD treatment focuses on keeping airways open long-term. First-line meds are long-acting bronchodilators: LABAs and LAMAs. These aren’t for emergencies - they’re daily maintenance. Inhaled steroids (ICS) are only added if you’ve had two or more flare-ups a year. Why? Because steroids don’t fix the core problem in COPD - they just help a subset of patients with mixed inflammation.
Pulmonary rehab helps COPD patients more than asthma patients. After a 12-week program, COPD patients typically walk 54 meters farther in six minutes. Asthma patients? Only 12 meters. Why? Because their baseline lung function is usually normal between attacks. They don’t need to relearn how to breathe - they just need to avoid triggers.
What about smoking?
Smoking is the biggest risk factor for COPD. Nine out of ten cases are caused by it. If you quit, you cut your disease progression in half. The Lung Health Study showed a 50% drop in decline after quitting - even if you’ve smoked for decades.
Smoking doesn’t cause asthma - at least not directly. Only about 20% of asthma cases are linked to smoking. But if you have asthma and smoke, your symptoms get worse, your meds stop working as well, and your risk of developing COPD skyrockets. That’s why doctors push hard for smoking cessation in asthma patients who smoke - it’s not just about lung health. It’s about preventing a second, irreversible disease.
What is Asthma-COPD Overlap Syndrome (ACOS)?
Not everyone fits neatly into one box. About 15-25% of people with obstructive lung disease have ACOS - a mix of both conditions.
These patients have the chronic cough and daily breathlessness of COPD, but also the eosinophilic inflammation and allergic triggers of asthma. Their sputum eosinophils are high (like asthma), but their airflow limitation doesn’t reverse much (like COPD). They’re more likely to end up in the ER - 1.8 times a year, on average - compared to 0.7 for asthma alone and 1.2 for COPD alone.
Treatment for ACOS often means using both asthma and COPD meds: a combination of LABA, LAMA, and ICS. But there’s no perfect formula. Evidence is still growing. That’s why accurate diagnosis matters more than ever.
What’s the long-term outlook?
Asthma has a much better survival rate. If you have moderate asthma, your 10-year survival chance is 92%. For moderate COPD? It drops to 78%.
That doesn’t mean asthma is harmless. Long-standing asthma - over 20 years - can lead to fixed airflow limitation in 15-20% of cases. That’s when asthma starts looking more like COPD. But even then, the inflammation pattern and response to treatment remain different.
COPD is the fourth leading cause of death in the U.S., killing about 152,000 people a year. Asthma kills about 3,500. That gap isn’t because asthma is “mild.” It’s because we’ve gotten better at managing it. Inhalers, action plans, and better monitoring have saved lives.
Can you have both?
Yes. And if you do, you need a different plan.
If you were diagnosed with asthma as a child and now, at 55, you’re smoking and your symptoms are getting worse, you might be developing COPD on top of it. Your doctor should check for both. A high-resolution CT scan can show emphysema - destroyed air sacs - which appears in 75% of COPD patients but only 5% of asthma patients.
Don’t assume your old asthma meds are enough. If you’re still wheezing after using your inhaler, or you’re coughing up phlegm every morning, it’s time to reevaluate.
What should you do if you’re unsure?
Write down your symptoms. When do they happen? What makes them better or worse? Do you have a daily cough? Do you feel better on some days? Have you ever smoked? How long? Bring this to your doctor.
Ask for spirometry. It’s simple, non-invasive, and the most reliable way to tell the difference. If your doctor says “it’s just asthma” without testing, get a second opinion.
Don’t wait for a crisis. COPD progresses silently. By the time you’re gasping for air, the damage is advanced. Asthma can be controlled - if you catch it early and treat it right.
Can asthma turn into COPD?
Asthma doesn’t directly turn into COPD, but long-term uncontrolled asthma - especially in smokers - can lead to permanent lung damage that looks like COPD. About 15-20% of people with asthma for more than 20 years develop fixed airflow limitation. This is called asthma-COPD overlap. It’s not the same as classic COPD, but it requires similar long-term management.
Is COPD curable?
No, COPD is not curable. The lung damage - whether from emphysema or chronic bronchitis - is permanent. But it’s manageable. Quitting smoking, using the right inhalers, doing pulmonary rehab, and avoiding infections can slow progression and let you live well for years. The goal isn’t to fix the lungs - it’s to keep them working as long as possible.
Can I use my asthma inhaler for COPD?
You might use the same type of inhaler - like albuterol - for quick relief in both conditions. But daily maintenance is different. Asthma relies on inhaled steroids to control inflammation. COPD doesn’t respond well to steroids unless you have frequent flare-ups. Using asthma meds for COPD without proper diagnosis can delay the right treatment and increase your risk of side effects like pneumonia.
Why do some people with asthma need biologics?
About 5-10% of asthma patients have severe, eosinophilic asthma that doesn’t respond to standard inhalers. These are people with high blood or sputum eosinophils, allergies, and frequent flare-ups. Biologics like omalizumab or mepolizumab target specific immune proteins to calm the inflammation. They’re injections given every few weeks and can cut flare-ups by 50% or more. They’re not for COPD.
Does breathing exercise help both conditions?
Pulmonary rehab - which includes breathing techniques, exercise, and education - helps COPD patients significantly. They gain strength, reduce breathlessness, and improve daily function. For asthma patients, the benefits are smaller because their lungs are usually healthy between attacks. Breathing exercises can help them manage anxiety during attacks, but they don’t improve lung function the same way. The real key for asthma is avoiding triggers and using preventer meds.
Bottom line: Know your lungs
Asthma and COPD are not interchangeable. One is often reversible. The other is progressive. One starts young. The other hits later. One responds to steroids. The other needs bronchodilators. One has a 92% 10-year survival rate. The other doesn’t.
If you’re struggling to breathe, don’t guess. Get tested. Know what you’re dealing with. The right diagnosis isn’t just about labels - it’s about getting the right treatment before it’s too late.


Michael Robinson
December 10, 2025So if asthma is like a storm you can躲过去, and COPD is like a slow leak in your tire... you're not fixing the tire, you're just patching it. And no matter how many patches, it's never going back to new.
Kathy Haverly
December 11, 2025Ugh. Another one of these "asthma is fine, COPD is death" articles. Did you even read the part where 20% of asthma patients end up with fixed airflow limitation? Or are you just here to scare people into buying more inhalers?
Haley P Law
December 12, 2025MY DAD HAD COPD AND HE STILL SMOKED UNTIL HE COULDN’T WALK TO THE FRIDGE 😭 I’M SO MAD AT HIM AND I MISS HIM SO MUCH 😔
Andrea DeWinter
December 13, 2025If you're over 40 and you've smoked even a little, get spirometry done. Seriously. Don't wait for the cough to get worse. I'm a nurse and I've seen too many people come in saying "I thought it was just asthma" and it's been COPD for years. Early detection = better quality of life. You don't need to be scared, just informed.
Steve Sullivan
December 14, 2025so like… asthma = temporary lock, copd = broken lock? i get it. also i smoke but i have asthma so i’m kinda scared now. anyone else feel like their lungs are just… tired? like your body’s like "bro i’ve been doing this for 30 years, can i nap now?"
George Taylor
December 14, 2025Interesting. But where’s the data on the cost of biologics? And the fact that most people can’t afford them? And that 87% of COPD patients are low-income smokers who can’t even get a doctor’s appointment? This article feels like it was written for people who already have good insurance and a primary care physician who listens.
ian septian
December 15, 2025Get tested. Don’t guess. That’s it.
Chris Marel
December 16, 2025I’m from Nigeria and we don’t have spirometers in most clinics. People here just get told "it’s asthma" and given inhalers. Many die quietly because no one knows the difference. Thank you for writing this. Maybe someone with resources will read it and do something.
Evelyn Pastrana
December 16, 2025So let me get this straight… if I had asthma as a kid and now I’m 50 and I smoke… I’m basically playing Russian roulette with my lungs? 😅 I guess I better stop buying cigarettes and start buying lung scans.
Katie Harrison
December 16, 2025I’m a 47-year-old who was diagnosed with asthma at 8. I quit smoking at 35. My doctor said I was lucky - my lungs were still mostly intact. But last year, my FEV1 dropped 18% in 12 months. Turns out I have ACOS. I didn’t know it was even a thing until I read this. I’m on LABA/LAMA/ICS now. It’s not perfect, but I can walk to the end of my driveway without stopping. If you’ve had asthma for decades and your meds aren’t working like they used to… don’t just up the dose. Ask for a spirometry repeat. And if your doctor says "it’s still asthma" - get a second opinion. Your lungs won’t wait.