Hemolysis Symptoms: What to Watch For and When to Act
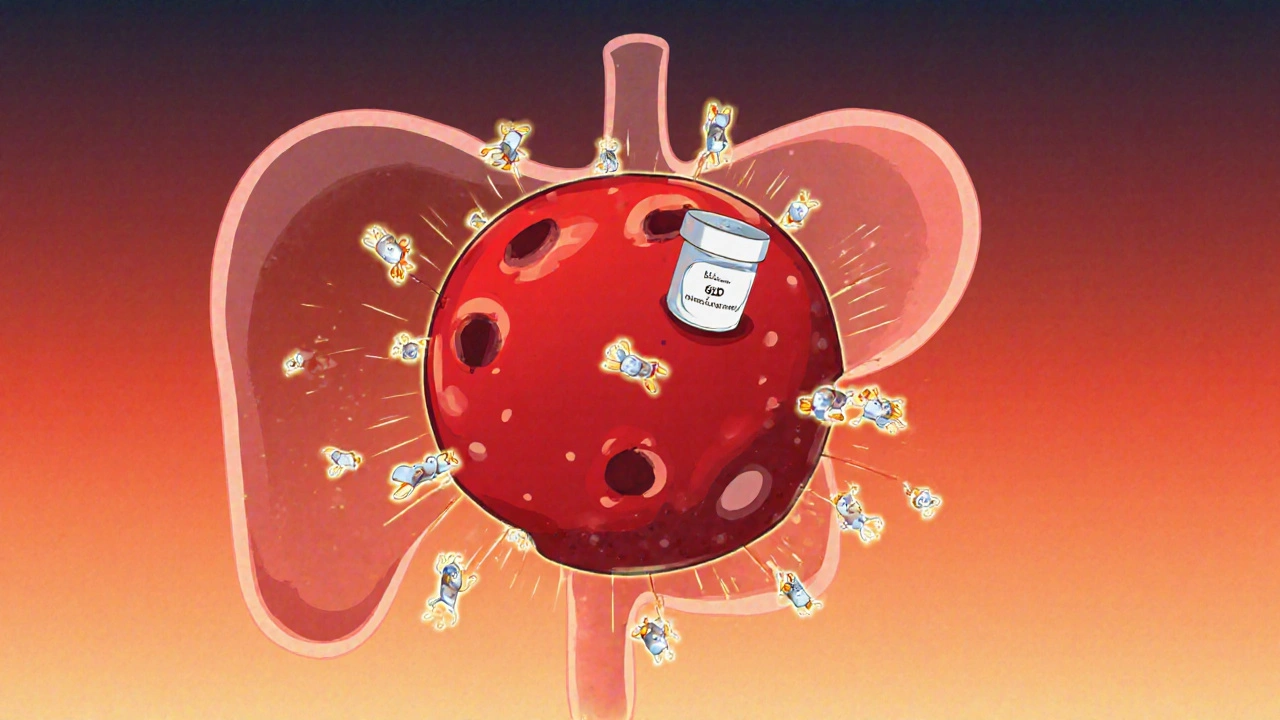
When hemolysis, the premature destruction of red blood cells happens, your body can’t replace them fast enough. This isn’t just a lab result—it’s a real, physical breakdown that shows up in how you feel. Hemolysis isn’t a disease itself, but a sign something’s wrong inside your bloodstream. It can come from medications, autoimmune problems, infections, or even inherited conditions like sickle cell or G6PD deficiency. When red blood cells burst open, they spill their contents into your blood, and that’s where the trouble starts.
One of the first things you might notice is jaundice, a yellowing of the skin and eyes caused by too much bilirubin. That yellow tint isn’t just from liver trouble—it’s from hemoglobin breaking down faster than your liver can process it. You might also see your urine turn dark, almost tea-colored, because the freed hemoglobin is being flushed out through your kidneys. Fatigue, shortness of breath, and a fast heartbeat are common too. These aren’t just "feeling tired" signs—they’re your body screaming that it’s not getting enough oxygen. Your spleen may even swell as it tries to clean up the damaged cells. In severe cases, you could develop abdominal or back pain, fever, or confusion. These aren’t random symptoms. They’re direct results of elevated bilirubin, a byproduct of red blood cell breakdown flooding your system.
What makes hemolysis tricky is that it can sneak up on you. Some people only notice it after a routine blood test shows low hemoglobin and high reticulocyte count. Others feel it right away—especially if they’ve just started a new drug like penicillin, cephalosporins, or even certain malaria meds. If you’re on a medication and suddenly feel worse, don’t assume it’s just a side effect. Ask about hemolysis. If you have a history of autoimmune disorders like lupus, or if you’ve had a recent infection, those are big red flags. The key is catching it early. Left unchecked, hemolysis can lead to kidney damage, heart strain, or even shock. You don’t need to be an expert to recognize the signs. If your skin looks yellow, your pee looks dark, and you’re unusually tired, get checked. The posts below cover real cases, drug triggers, and how doctors confirm this condition—so you know exactly what to look for and what questions to ask.
Hemolytic Anemia from Medications: Recognizing Red Blood Cell Destruction
Drug-induced hemolytic anemia is a rare but dangerous condition where medications trigger the immune system to destroy red blood cells. Recognizing symptoms like fatigue, jaundice, and dark urine-and knowing which drugs are most likely to cause it-can save lives.