16 Nov 2025
- 13 Comments
More than 1 in 10 adults in Australia has gallstones. But here’s the thing-most of them never even know it. The pain doesn’t come from the stones themselves. It comes when one gets stuck. That’s when your body screams for help.
What Happens When a Gallstone Gets Stuck?
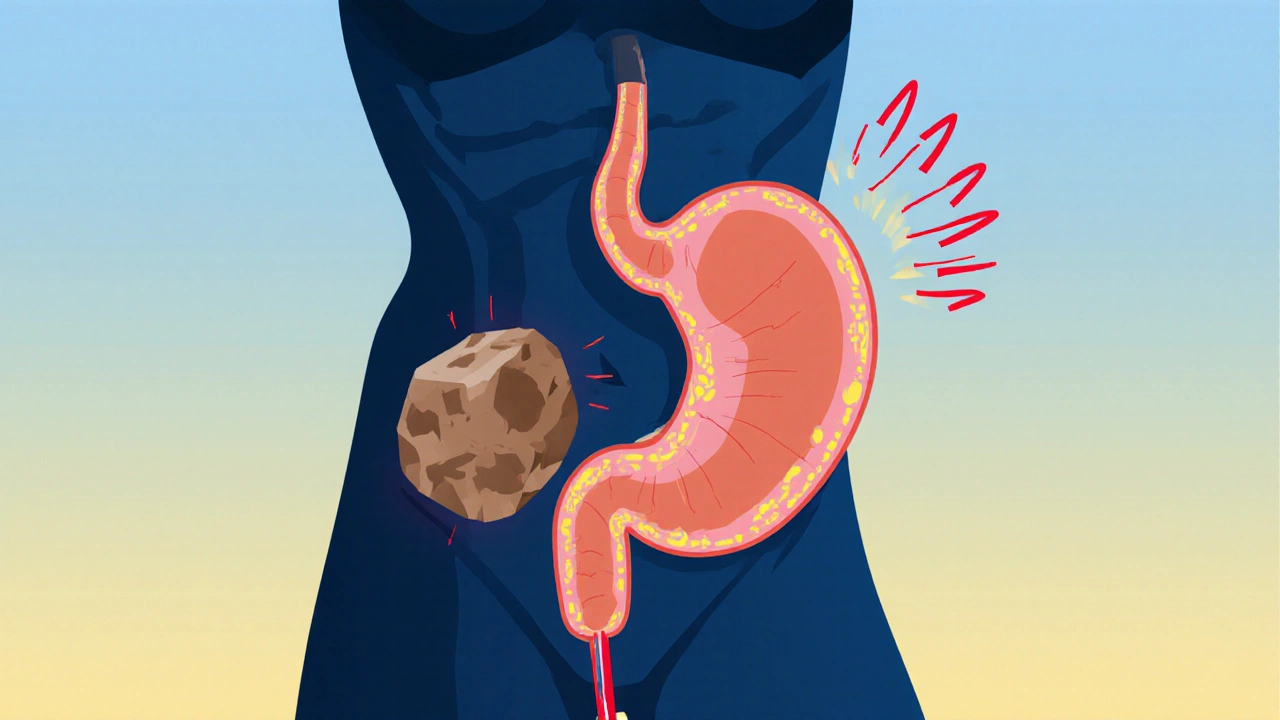
Imagine your gallbladder is a small storage tank for bile, the fluid your liver makes to digest fat. When you eat, it squeezes out bile through a narrow tube called the cystic duct. If a stone blocks that tube-even briefly-you get biliary colic.
This isn’t a dull ache. It’s a sharp, steady pain under your right ribs or in the middle of your belly. It hits fast, peaks within an hour, and lasts 1 to 5 hours. It doesn’t get better when you burp, pass gas, or throw up. You can’t just walk it off. And it doesn’t come with fever or jaundice-that’s the next step.
Up to 90% of people who have one episode of biliary colic will have another within 10 years. Two-thirds will be back in pain within just two years. That’s not luck. That’s the pattern. And each time it happens, the risk of something worse goes up.
When It Turns Serious: Cholecystitis
If the stone stays stuck for more than a few hours, your gallbladder starts to swell and inflame. That’s acute cholecystitis. Now you’re not just in pain-you’re sick.
You’ll likely have a fever, nausea, and your right upper belly will be tender to the touch. Your skin might turn yellow if the stone moves into the main bile duct. That’s called jaundice. You might even get pancreatitis if the stone blocks the pancreatic duct.
One in five people with biliary colic ends up here. And if you don’t get treated, your gallbladder can rupture. That’s life-threatening. The NHS says 20-30% of people with untreated symptomatic gallstones end up in emergency care within five years.
Doctors don’t wait. If you have cholecystitis, surgery should happen within 72 hours. Delaying increases the chance you’ll need open surgery instead of the minimally invasive kind. And open surgery means weeks of recovery-not days.
What Are Gallstones Made Of?
Not all stones are the same. In Western countries like Australia, about 80% are cholesterol stones. They form when your bile has too much cholesterol and not enough bile salts to keep it dissolved. The rest are pigment stones, made of bilirubin, a waste product from broken-down red blood cells.
Women are 2-3 times more likely to get them than men. Why? Estrogen increases cholesterol in bile and slows gallbladder emptying. Pregnancy, birth control pills, and hormone therapy all raise the risk. So do obesity, rapid weight loss, diabetes, and being over 40. Hispanic Australians have a 45% higher chance than non-Hispanic people.
And here’s the kicker: you can have dozens of stones the size of peas-or one big one like a golf ball. Size doesn’t predict symptoms. It’s all about location.
Can You Dissolve Gallstones Without Surgery?
You’ve probably heard about pills that dissolve stones. Ursodeoxycholic acid (UDCA) is real. It works-sometimes. But only for small, pure cholesterol stones. Success rates? 30-50% after 6 to 24 months of daily pills. And even if it works, half the people get stones back within five years.
Shockwave therapy (lithotripsy) used to be a popular option. It breaks stones into tiny pieces so they can pass. But it only works for single stones under 20mm. It’s messy, expensive, and rarely used anymore because recurrence is so high.
There’s also a new FDA-approved option for high-risk patients: endoscopic ultrasound-guided gallbladder drainage. It’s not a cure-it’s a bridge. It drains the gallbladder through a tiny tube, relieving pressure and infection without removing the organ. It’s for people too sick for surgery right now. But it’s not a long-term fix.
For most people, these aren’t real alternatives. They’re delays. And delays cost you time, comfort, and safety.
Why Laparoscopic Cholecystectomy Is the Gold Standard
Remove the gallbladder. That’s the cure. And the best way to do it? Laparoscopic cholecystectomy.
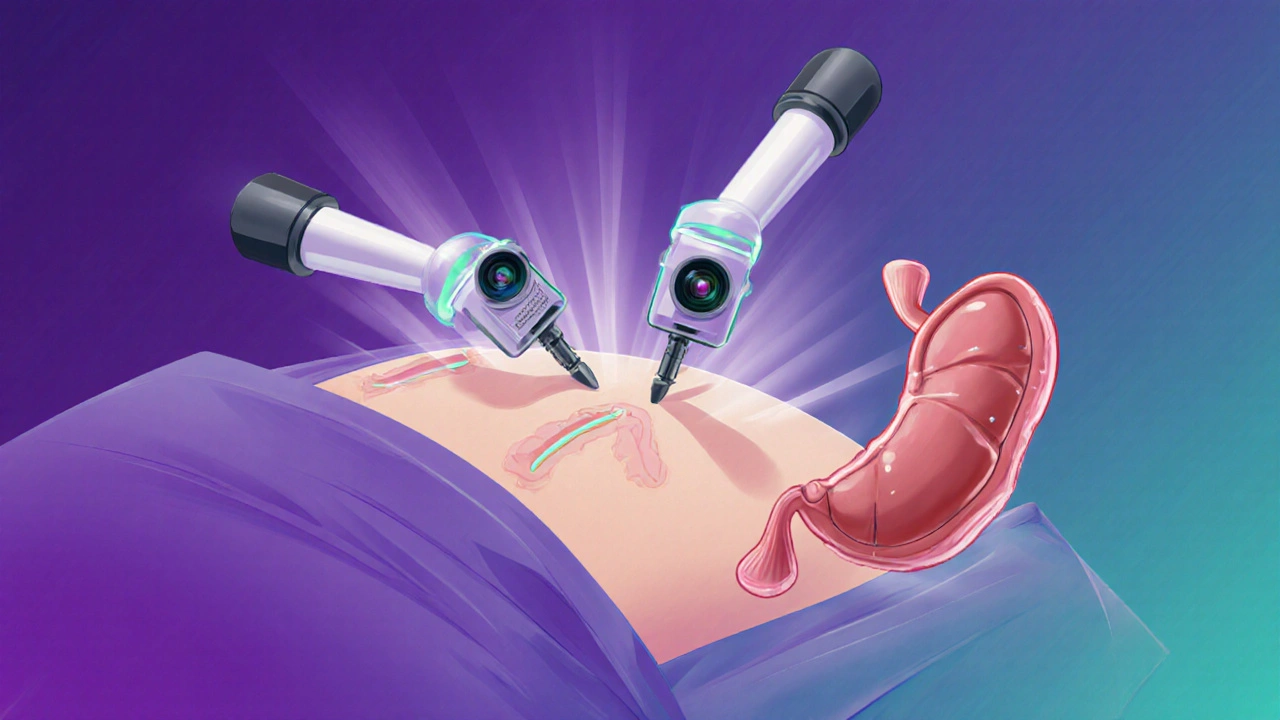
This isn’t a big cut. Surgeons make 3-4 tiny holes in your belly. They insert a camera and tools. They clip the ducts, cut the gallbladder loose, and pull it out. The whole thing takes 45 to 60 minutes. Most people go home the same day.
Compare that to open surgery: a 6-inch cut, 4-5 days in hospital, 30 days to recover. Laparoscopic surgery has a 95% patient satisfaction rate. Complication rates? Below 2% in experienced hands.
Recovery is fast. Walk within 4 hours. Drink liquids within 6. Eat light meals by dinner. Back to work in a week. No heavy lifting for 4-6 weeks. That’s the standard.
One woman in Cleveland Clinic’s 2023 patient story had 17 episodes of biliary colic over 18 months. After surgery, her pain vanished in 10 days. She was back to hiking in two weeks.
Who Shouldn’t Have Surgery?
Surgery isn’t risk-free. For healthy people under 75, the risk of dying within 30 days is about 0.1%. For someone over 75 with three or more chronic conditions-like heart disease, diabetes, or lung problems-that jumps to 2.8%.
That’s why doctors don’t rush. If you’re older and frail, they might try to manage symptoms with diet and pain control. But even then, the risk of complications like infection or bile duct injury stays high. Many end up in the hospital anyway.
There’s no magic age cutoff. It’s about your overall health, not your birthday. A 78-year-old who walks daily and manages their blood pressure might be a better candidate than a 65-year-old with uncontrolled diabetes.

What About Side Effects After Surgery?
Most people feel better than they have in years. But not everyone.
About 12% have ongoing diarrhea after surgery. It’s called post-cholecystectomy syndrome. Your body suddenly has to handle bile differently-no gallbladder to store it. That can make digestion less efficient, especially after fatty meals.
Another 6% get persistent pain. That’s not normal. It could mean a leftover stone, a bile leak, or even something unrelated like IBS. You need imaging and tests to find out.
On Reddit, 82% of people who had the surgery said their quality of life improved. The rest? Mostly those who waited too long or had undiagnosed problems.
What’s Next for Gallstone Treatment?
Surgeons are now using single-incision laparoscopic surgery (SILS)-one small cut instead of three. It leaves less scarring. But it’s harder to do. Complication rates are 20% higher than standard laparoscopy. It’s not the new standard yet.
Enhanced Recovery After Surgery (ERAS) protocols are making recovery faster. Eat before surgery. Don’t fast for 12 hours. Start walking within hours. These simple changes cut hospital stays by 30% and readmissions by 25%.
And the market is growing. With obesity rates rising and populations aging, more people will need this surgery. In the U.S., 700,000 gallbladder removals are done every year. That’s a $6.2 billion industry.
But here’s the bottom line: despite new tech, cholecystectomy remains the only reliable cure. Dissolving stones? Temporary. Draining the gallbladder? A stopgap. Surgery? Permanent.
What Should You Do If You Have Gallstones?
If you’ve been diagnosed with gallstones but never had symptoms-do nothing. Monitor. Eat healthy. Don’t lose weight too fast.
If you’ve had one episode of biliary colic? Talk to a surgeon. Don’t wait for the next one. The odds of recurrence are high. And each episode raises your risk of emergency surgery.
If you’re in pain right now-with fever, nausea, or jaundice? Go to the ER. Don’t wait. Don’t try to tough it out. This isn’t a stomach bug. It’s a medical emergency.
And if your doctor says, ‘Let’s wait and see’-ask why. If they’re not offering surgery as the main option, they’re not following current guidelines. The AAFP, SAGES, and Merck Manual all agree: for symptomatic gallstones, cholecystectomy is the standard.
You don’t need to suffer through 17 episodes like that woman in Cleveland. You don’t need to risk a ruptured gallbladder. You don’t need to be stuck in the hospital for weeks.
Surgery isn’t scary when you understand it. And it’s the only thing that gives you back your life.
Can gallstones go away on their own?
No. Gallstones don’t dissolve or disappear without treatment. Silent stones may never cause problems, but once they start causing pain, they won’t fix themselves. Medications like ursodeoxycholic acid can dissolve small cholesterol stones in some people, but only after months of daily pills-and even then, half the people get them back within five years. Surgery is the only permanent solution.
Is gallbladder surgery dangerous?
For healthy people under 75, the risk of serious complications or death is less than 2%. Laparoscopic cholecystectomy is one of the safest common surgeries. The biggest risks come from waiting too long-delaying surgery increases the chance of infection, bile duct injury, or needing open surgery. For older adults with multiple health issues, risks rise, so doctors weigh benefits carefully.
What happens to digestion after gallbladder removal?
Your liver still makes bile, but without the gallbladder to store it, bile flows continuously into your intestine. That can make digestion of fatty foods less efficient. About 12% of people get temporary diarrhea after surgery, especially after greasy meals. Most adjust within weeks. Eating smaller, low-fat meals helps. Long-term, most people digest food normally.
How long does recovery take after gallbladder surgery?
With laparoscopic surgery, most people go home the same day or the next. You can walk within hours and eat light meals within 6 hours. Return to desk work in 3-5 days. Full recovery, including lifting heavy objects, takes 4-6 weeks. Open surgery requires 4-6 weeks in hospital and up to 3 months to fully recover.
Do I need to change my diet after gallbladder removal?
You don’t need a strict diet, but you’ll feel better avoiding large, fatty meals right after surgery. Your body needs time to adjust to constant bile flow. Start with small portions of lean protein, vegetables, and whole grains. Avoid fried foods, creamy sauces, and heavy desserts for the first few weeks. Most people return to their normal diet without issues after 4-6 weeks.
Can I get gallstones again after surgery?
No. Once your gallbladder is removed, you can’t get gallstones again. The stones form inside the gallbladder. Without it, there’s no place for them to form. Some people report ongoing pain after surgery, but that’s not from new stones-it’s from other issues like bile duct problems, IBS, or undiagnosed conditions. If pain continues, further testing is needed.
Why do some people still have pain after gallbladder surgery?
About 6% of people experience ongoing pain after surgery. This is called post-cholecystectomy syndrome. It’s not caused by new stones. Possible reasons include bile duct stones missed during surgery, bile leakage, scar tissue narrowing the bile duct, or unrelated conditions like acid reflux or IBS. If pain lasts more than a few weeks, you need imaging like an ultrasound or MRCP to find the cause.
Is it safe to wait and see if gallstones cause symptoms?
Only if you’ve never had symptoms. Once you’ve had even one episode of biliary colic, your chance of another is over 90% within 10 years. Waiting increases your risk of emergency surgery, infection, or pancreatitis. Most experts recommend surgery after the first symptomatic episode-it’s safer, easier, and gives you back your life faster.

Robert Merril
November 17, 2025So let me get this right you cut out a perfectly good organ because sometimes it gets clogged like a drain in my kitchen sink? I mean yeah I get the pain but why not just try not eating grease for a month first? My abuela did it and she lived to 98
Noel Molina Mattinez
November 17, 2025They say surgery is the only cure but what if you just stop eating meat and dairy for a while and see what happens
Roberta Colombin
November 18, 2025Thank you for sharing this clear and compassionate overview. Many people live in fear of surgery without understanding how safe and life-changing it can be. I’ve seen patients go from bedridden to hiking again in weeks. You are not alone in this journey. There is support. There is hope.
Julie Roe
November 19, 2025I had my gallbladder out three years ago after 14 episodes of pain so bad I thought I was having a heart attack and honestly I can’t believe I waited this long. I used to plan my entire life around when I could get to a bathroom or when I could eat something safe. Now I eat tacos at midnight and go for runs on weekends. The diarrhea thing? Yeah it happened for like two weeks and then it just stopped. My body figured it out. The biggest thing I wish someone had told me is that you don’t need to suffer like this. It’s not normal. It’s not aging. It’s your body screaming and nobody listens until it breaks. Don’t be me. Get it checked.
jalyssa chea
November 19, 2025They say surgery is the only cure but what about the government hiding the truth about gallstones and how they’re caused by fluoride in the water and GMOs? I read a guy on YouTube who cured his with apple cider vinegar and moon phases. Also why is the NHS mentioned like they’re some kind of authority? They ration everything. They probably want you to suffer so they can save money
Gary Lam
November 20, 2025Bro I had the surgery last year and now I’m basically a new person. I used to dread birthdays because I couldn’t eat cake. Now I eat cake. I eat butter. I eat fried chicken. I’m free. Also the doctor said I could drink alcohol again. I didn’t think I’d ever be able to have a beer after dinner again. This isn’t just a procedure. It’s a liberation.
Peter Stephen .O
November 20, 2025Let’s talk about bile flow like it’s a river that used to have a dam and now it’s wide open and flowing 24/7. Your liver’s like hey I’m still making juice but no more storage unit so now everything’s just chillin’ in your intestines. First week? Yeah it’s wild. You feel like your guts are throwing a rave. But your body? It’s a genius. It adapts. You learn what foods are chill and what ones start a riot. And then boom - you’re back to life. No more panic attacks when you eat pizza. No more hiding in the bathroom. Just freedom. And yeah maybe you gotta skip the double cheeseburger once in a while but hey that’s not a sacrifice. That’s just upgraded living.
Andrew Cairney
November 22, 2025Wait so you’re telling me they’re just gonna cut out my gallbladder like it’s some kind of defective part? What if they don’t get it all? What if they leave a stone behind and it starts growing inside me like some kind of alien egg? I saw a video where a guy had a cyst in his liver that turned into a tumor because the doctors missed it. And now they’re pushing this like it’s a spa day? I’m not signing anything until I get a second opinion from a guy who doesn’t work for Big Pharma. 😈
Rob Goldstein
November 23, 2025From a clinical perspective, the key point here is that cholecystectomy for symptomatic cholelithiasis is supported by Level I evidence across multiple guidelines including SAGES and AAFP. The natural history of recurrent biliary colic carries a significant risk of progression to acute cholecystitis, choledocholithiasis, and pancreatitis. The morbidity and mortality associated with emergency cholecystectomy are substantially higher than elective procedures. The 95% satisfaction rate post-laparoscopic cholecystectomy is not anecdotal - it’s validated in large cohort studies. The real question isn’t whether to operate - it’s why we delay.
vinod mali
November 24, 2025I had this in India. Doctor said wait. I waited. Then I got sick. Emergency. Open surgery. Took 3 weeks to walk. Now I eat everything. No pain. But please don’t wait like me. Talk to a surgeon early. It’s not scary. It’s smart.
Jennie Zhu
November 26, 2025The empirical data supporting early laparoscopic cholecystectomy for symptomatic gallstone disease is robust and well-documented in peer-reviewed surgical literature. Delayed intervention increases the likelihood of complications requiring extended hospitalization, higher resource utilization, and elevated perioperative risk. The standard of care, as articulated by authoritative clinical guidelines, unequivocally supports timely surgical referral following the first symptomatic episode.
Kathy Grant
November 28, 2025There’s something so deeply human about this whole thing - how we ignore our bodies until they scream. We treat pain like it’s a personal failure. Like if we just ate better or meditated more or waited longer, it would go away. But the gallbladder doesn’t care about your willpower. It doesn’t care about your diet trends or your detox teas. It just holds bile. And when it gets blocked? It doesn’t whisper. It roars. And the bravest thing you can do isn’t to tough it out - it’s to say, ‘I’m done listening to my body beg.’ And then you say yes to healing. Even if it means letting go of a part of yourself. Sometimes healing isn’t about adding something. Sometimes it’s about removing what’s been holding you back.
Dave Feland
November 29, 2025While the article presents itself as authoritative, it conspicuously omits any mention of the fact that the laparoscopic cholecystectomy procedure was popularized by French surgeons in the 1980s, who were initially ridiculed by the American surgical establishment. This is not medicine - it’s institutional inertia. The fact that 700,000 procedures are performed annually in the U.S. alone suggests a profitable industry, not a medical necessity. The true cause of gallstones? Insulin resistance and industrial seed oils - not estrogen. The article is a corporate brochure disguised as patient education.