Opioid Dependence: Signs, Risks, and What You Need to Know
When people talk about opioid dependence, a physical and psychological condition where the body relies on opioid drugs to function normally. Also known as opioid addiction, it doesn’t always mean someone is abusing drugs—it can happen after just a few weeks of taking prescribed painkillers like oxycodone, hydrocodone, or morphine. This isn’t weakness. It’s biology. Opioids bind to receptors in your brain and spinal cord, dulling pain but also triggering dopamine release. Over time, your brain stops making its own natural painkillers and feels normal only when opioids are present.
One of the most overlooked dangers of long-term opioid use is opioid-induced adrenal insufficiency, a condition where the body stops producing enough cortisol, the hormone that helps you handle stress. Without enough cortisol, even a minor illness like the flu can turn life-threatening. Symptoms like constant fatigue, nausea, low blood pressure, and dizziness are often mistaken for depression or general tiredness. If you’ve been on opioids for more than a few months and feel worse when you’re sick, this could be why.
Withdrawal isn’t just about cravings or muscle aches. It’s your nervous system screaming to reset after being suppressed for too long. Symptoms can include sweating, insomnia, diarrhea, anxiety, and intense pain returning stronger than before. Many people stop treatment because withdrawal feels unbearable—but it doesn’t have to be. Tapering slowly under medical supervision makes a huge difference. And it’s not just about stopping. It’s about rebuilding your body’s ability to manage pain and stress naturally.
Dependence doesn’t always look like street drugs or overdose. It shows up in someone who can’t sleep without their pill, who skips work because they’re too nauseous to get out of bed, or who hides their prescriptions because they’re scared of being judged. The real problem isn’t the drug—it’s the lack of awareness. Most patients aren’t told about adrenal risk, withdrawal timelines, or alternatives like non-opioid pain management. That’s changing, slowly. But you need to know the signs before it’s too late.
What you’ll find below are real, practical articles that cut through the noise. From how opioids quietly shut down your adrenal glands to how to spot dangerous interactions with other meds, these posts give you the facts you won’t hear at the pharmacy counter. No fluff. No fearmongering. Just what you need to protect yourself—or someone you care about.
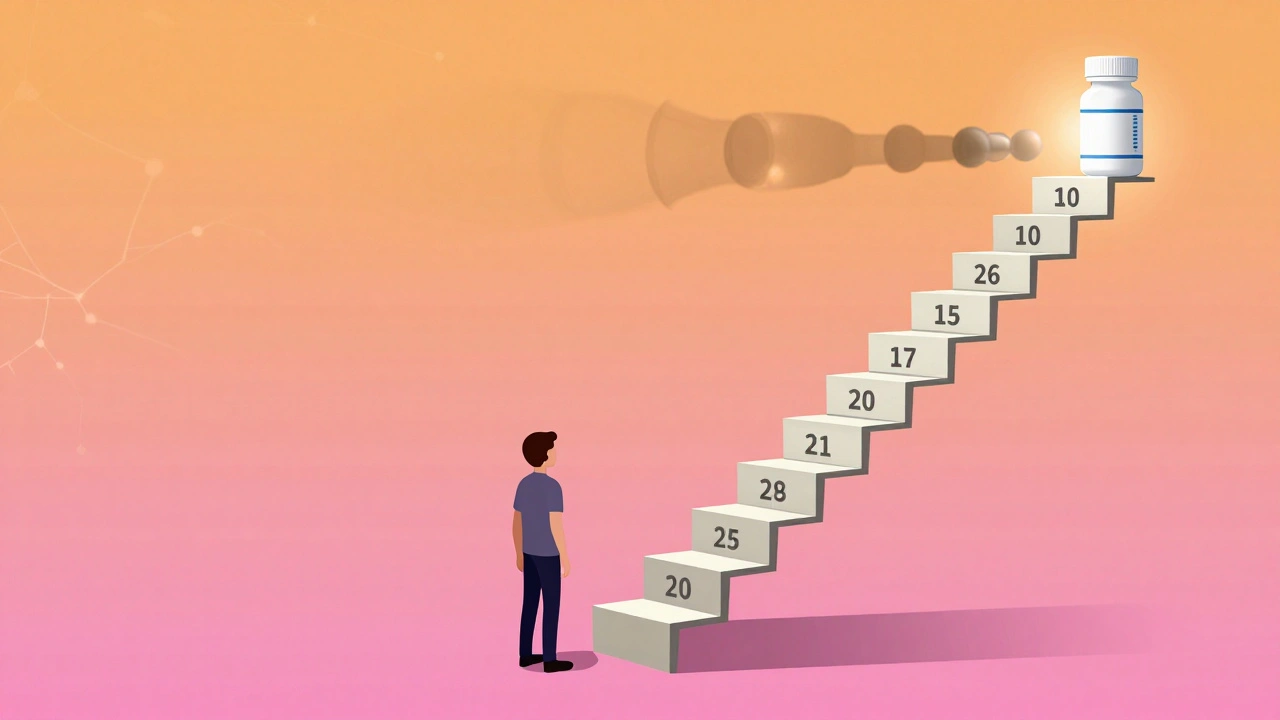
Opioid Tolerance: Why Your Pain Medication Dose Keeps Going Up
Opioid tolerance means your body needs higher doses for the same pain relief. It’s not addiction - but it can lead to dangerous outcomes if not managed carefully. Learn why doses increase and how to stay safe.