3 Dec 2025
- 12 Comments
Opioid Dose Safety Checker
How This Tool Works
This tool helps you understand your opioid dose safety based on CDC guidelines. It calculates morphine milligram equivalents (MME), shows overdose risks after tolerance loss, and provides evidence-based safety recommendations.
Dose Calculator
Critical Warning
If you've been off opioids for more than 1 week, restarting at your previous dose carries a 74% overdose risk (CDC data).
Key Safety Tip: If returning to opioids after stopping, start with 25% of your previous dose and increase only under medical supervision.
Results
Dose Summary
CDC Safety Recommendations
- Non-opioid pain management
- Medication rotation
- Physical therapy
- Cognitive behavioral therapy
When you first start taking opioids for pain, they work like magic. The ache fades, you can sleep, move better, even smile again. But after a few weeks or months, something changes. The same dose doesn’t help as much. You feel like you need more - and your doctor agrees. That’s not a failure. It’s not weakness. It’s opioid tolerance.
What Exactly Is Opioid Tolerance?
Opioid tolerance happens when your body gets used to the drug. It’s not about addiction. It’s not about craving. It’s biology. Your brain and nervous system adapt to the constant presence of opioids. The receptors that once responded strongly to the medication start to shut down or pull back. This is called receptor desensitization. Over time, your body needs higher doses to get the same pain relief you had at first.
The U.S. Food and Drug Administration defines it simply: exposure to opioids causes changes that reduce their effects over time. That’s it. No judgment. Just science. And it doesn’t happen the same way for everyone. Some people notice it after a few weeks. Others stay stable for months. Genetics, metabolism, how often you take it, and even your pain condition all play a role.
Why Does This Happen Inside Your Body?
At the center of it all is the mu-opioid receptor - the main target for drugs like oxycodone, hydrocodone, and morphine. When opioids bind to these receptors, they trigger pain relief and sometimes a sense of calm or euphoria. But when that happens over and over, your cells respond by:
- Reducing the number of receptors on the surface of nerve cells (downregulation)
- Changing how the receptors signal inside the cell (desensitization)
- Activating inflammatory pathways like TLR4 and NLRP3, which make your nervous system more reactive to pain
It’s like turning down the volume on a speaker that’s always blaring. At first, the sound is loud and clear. But if it never stops, your ears adjust. You need to turn the volume higher just to hear it the same way. Your nervous system does the same thing.
And here’s the tricky part: tolerance doesn’t develop evenly. You might lose sensitivity to pain relief faster than you lose sensitivity to drowsiness or nausea. That means you could be taking more just to manage pain - but still feel dangerously sleepy or have slowed breathing at the same dose. That’s why dose increases can be risky.
Tolerance vs. Dependence vs. Addiction
People mix these up all the time. Let’s clear it up.
- Tolerance = you need more to get the same effect.
- Dependence = your body relies on the drug to function normally. If you stop, you get withdrawal - sweating, shaking, nausea, anxiety.
- Opioid Use Disorder (OUD) = when using opioids causes serious problems in your life - job loss, relationship issues, health decline, or risky behavior.
You can have tolerance without dependence. You can have dependence without addiction. But tolerance often leads to dependence. And dependence, without support, can spiral into addiction. The Centers for Disease Control and Prevention (CDC) makes this distinction because it matters for treatment. You don’t treat tolerance like addiction. You manage it differently.

Why Dose Increases Are a Red Flag
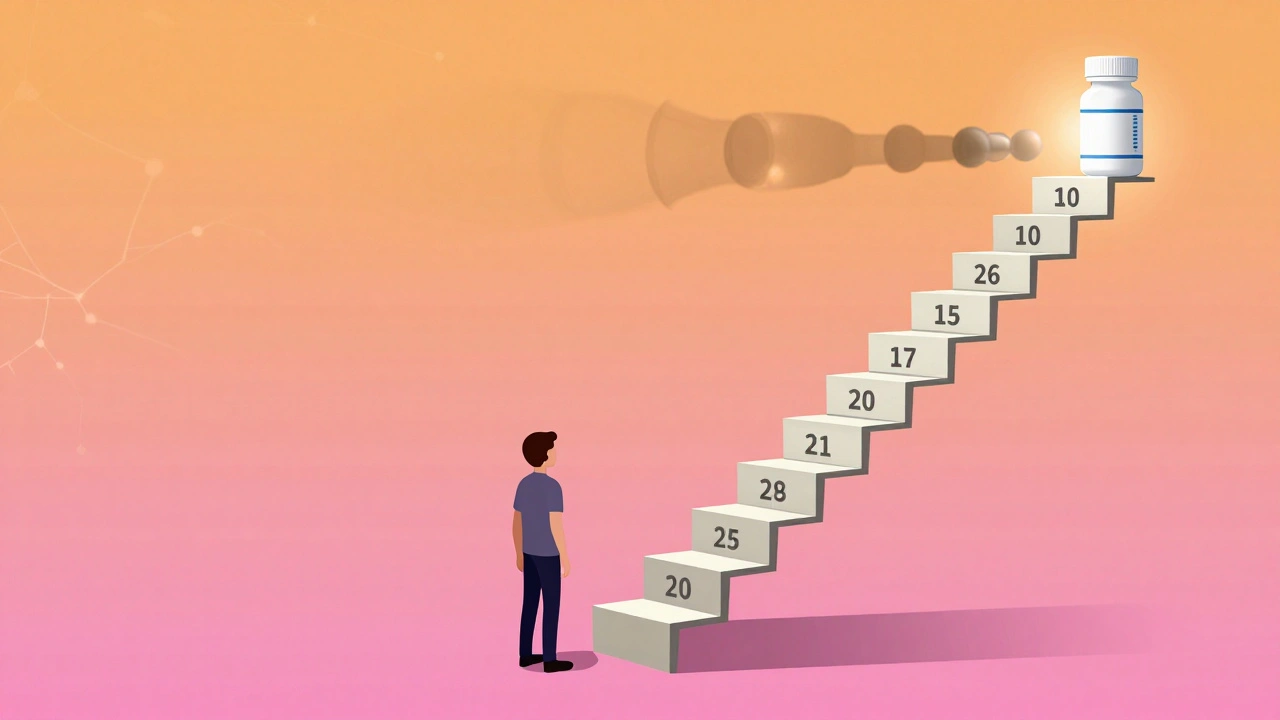
Increasing your opioid dose doesn’t always mean better pain control. In fact, the CDC found that about 30% of people on long-term opioids need higher doses within the first year. But after that, the benefits drop off sharply. Higher doses mean more side effects - constipation, dizziness, confusion, breathing problems - without much extra pain relief.
And here’s the hard truth: once you’re on a high dose, going back down is hard. Your body has adapted. You might feel worse without it. But staying on high doses increases your risk of overdose - especially if you’re also using alcohol, benzodiazepines, or sleep aids.
That’s why the CDC recommends that before crossing 50 morphine milligram equivalents (MME) per day, your doctor should pause. Ask: Is this still working? Are there other options? Are we just chasing a number instead of real improvement in your life?
The Dangerous Myth: "I Need More Because It’s Not Working"
Many patients believe that if the medicine isn’t doing enough, they just need more. That logic makes sense - until it doesn’t. Opioids don’t fix the root cause of pain. They mask it. And over time, your nervous system can become more sensitive to pain itself. This is called opioid-induced hyperalgesia. You’re taking more to fight pain - but the drug is actually making your body more reactive to it.
Studies show that around 40% of chronic pain patients on long-term opioids report reduced effectiveness within six months. That’s not a personal failure. It’s a known physiological response. The solution isn’t always a higher dose. Sometimes, it’s switching to a different medication, adding physical therapy, or using non-opioid pain relievers like gabapentin or antidepressants that target nerve pain.
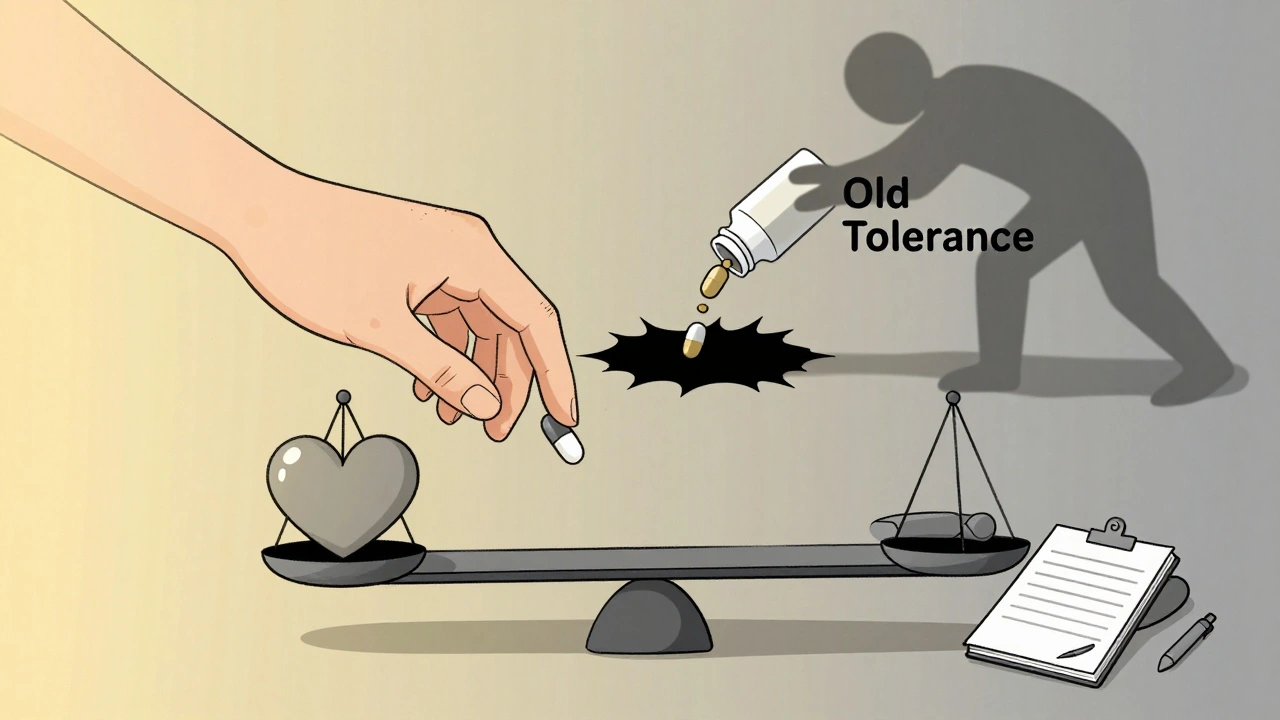
Tolerance Can Disappear - And That’s Deadly
This is one of the most underreported dangers. If you stop taking opioids - even for a short time - your tolerance drops. Fast. A week off. A month in rehab. A stint in jail. Your body forgets how to handle the drug.
Now, if you go back to your old dose? You could overdose. Your system isn’t prepared. That’s why 74% of fatal opioid overdoses among people with opioid use disorder happen within the first few weeks after release from incarceration. And 65% of overdose deaths in recovery involve people returning to their previous dose without adjusting.
Doctors and treatment centers now warn patients: "Your tolerance is lower now. Start with a fraction of what you used to take." That message saves lives. But too few people hear it.
What Can Be Done?
There’s no magic fix - but there are smarter ways forward.
- Medication rotation: Switching from one opioid to another (like from oxycodone to methadone) can reset tolerance in some cases. This isn’t always easy, and it requires careful monitoring.
- Combination therapies: Early trials are testing low-dose naltrexone (a drug that blocks opioid receptors) alongside opioids. In some cases, this slowed tolerance development by 40-60%. It’s not standard yet, but it’s promising.
- Non-opioid options: Physical therapy, cognitive behavioral therapy, acupuncture, and even certain antidepressants can reduce pain without the risk of tolerance.
- Regular reassessment: Every 3-6 months, ask: Is this still helping? Am I moving better? Sleeping better? Or am I just taking pills to avoid withdrawal?
And if you’ve been off opioids for any length of time - even a few days - never go back to your old dose. Start low. Go slow. Talk to your doctor. Your life depends on it.
What’s Next for Opioid Pain Management?
Researchers are now looking at how inflammation drives tolerance. New drugs targeting TLR4 and NLRP3 pathways are in early testing. The FDA is pushing for new pain medications that work without causing tolerance. That’s the holy grail - pain relief without the climb.
But until then, the best tools we have are awareness and caution. Tolerance isn’t a flaw. It’s a signal. A sign that your body is trying to protect itself. The goal isn’t to fight it with higher doses. It’s to understand it - and respond with smarter, safer choices.
Is opioid tolerance the same as addiction?
No. Tolerance means you need more of the drug to get the same effect. Addiction, or opioid use disorder, means you can’t control your use despite harm - like losing your job, relationships, or health. You can have tolerance without addiction, and addiction without tolerance, but they often happen together.
Can I stop taking opioids if I’ve developed tolerance?
Yes, but not abruptly. Stopping suddenly can cause severe withdrawal. Work with your doctor to create a slow, safe tapering plan. Even if you’ve been on high doses, reducing slowly over weeks or months can help your body adjust without dangerous symptoms.
Why do some people develop tolerance faster than others?
Genetics play a big role - especially variations in the OPRM1 gene, which controls opioid receptors. Metabolism, liver function, age, and how often you take the drug also matter. Some people develop tolerance in weeks. Others stay stable for months. There’s no one-size-fits-all timeline.
Does tolerance mean I’m addicted to opioids?
Not at all. Many people with chronic pain develop tolerance while still using opioids safely and as prescribed. Addiction involves compulsive use, loss of control, and harm to your life. Tolerance is a physical change. Addiction is a behavioral and psychological condition.
What should I do if my pain medicine isn’t working anymore?
Don’t increase the dose on your own. Talk to your doctor. Ask about non-opioid options like physical therapy, nerve blocks, or medications like gabapentin. Consider a pain specialist. Sometimes, switching opioids or adding a non-opioid treatment can restore relief without raising your dose.
Is it safe to use opioids again after being off them for a while?
No - not at your old dose. Your tolerance drops quickly after stopping. Even a week off can make you vulnerable to overdose. If you’re returning to opioids after a break - whether from rehab, jail, or just stopping - start with a very low dose and increase slowly under medical supervision.
Can I avoid opioid tolerance altogether?
It’s hard to avoid completely if you’re taking opioids regularly. But you can slow it down. Use the lowest effective dose. Take breaks when possible. Combine opioids with non-drug treatments. Avoid using them for long-term chronic pain unless absolutely necessary. The goal isn’t to never use them - it’s to use them wisely.
Final Thoughts
Opioid tolerance isn’t a sign you’re doing something wrong. It’s a sign your body is doing exactly what it’s supposed to do - adapting. But in a world where fentanyl is 50 times stronger than heroin, and street drugs vary wildly in potency, that adaptation can turn deadly. The key isn’t to fight tolerance with more pills. It’s to understand it, respect it, and plan around it. Your safety - and your life - depends on it.

Rudy Van den Boogaert
December 3, 2025Been on opioids for 8 years now. Tolerance hit me hard at year 3. Didn't realize it was biology until my pain specialist sat me down and explained receptor downregulation. It's not weakness. It's just your body being smart. I switched to methadone and it reset things enough to keep me functional. No magic fix, but knowledge is power.
Shofner Lehto
December 4, 2025This is one of the clearest explanations of opioid tolerance I've ever read. No fluff, no judgment, just science. Doctors need to give patients this kind of info upfront, not after they've been stuck on escalating doses for years.
Libby Rees
December 5, 2025I appreciate how you separated tolerance from addiction. So many people conflate the two and it makes patients feel guilty for needing medication. This clarity matters.
Jessica Baydowicz
December 5, 2025My mom’s been on opioids since her back surgery. She cried when she found out her dose wasn’t working because she thought she was failing. This post? It gave her peace. Thank you for writing this.
Gillian Watson
December 6, 2025Had a cousin overdose after jail. He went back to his old dose. Nobody told him tolerance drops fast. This needs to be shouted from rooftops.
Bill Wolfe
December 6, 2025Oh, here we go again with the ‘tolerance is normal’ narrative. 🤦♂️ Let’s not pretend this isn’t just the pharmaceutical industry’s way of keeping people hooked. You think they care about your receptors? They care about your refill schedule. The FDA? They’re on the payroll. Tolerance isn’t biology-it’s a business model disguised as science. 🧪💸
Benjamin Sedler
December 6, 2025So what you’re saying is, if I stop for a week, my body forgets how to handle the drug? That’s wild. So basically, if I get arrested, I should bring my own low-dose starter pack? 😏
michael booth
December 7, 2025Thank you for this. I’ve been a chronic pain patient for 12 years. I’ve tried everything. Opioids were the only thing that let me hold my daughter. But I’ve learned to use them sparingly, with PT and CBT. It’s not perfect, but it’s sustainable. You’re not alone.
Gareth Storer
December 7, 2025So… if I’m on 100 MME and I get locked up for a month, then I go back to my old dose… I’m basically doing a slow-motion suicide? Cool. Thanks for the heads up, I guess.
Yasmine Hajar
December 8, 2025My brother died last year. He was in rehab. Came out. Took his old dose. Didn’t wake up. This isn’t theoretical. This is real. Please, if you’re reading this and you’ve been off opioids-even for a few days-start at 1/4 of what you used to. Don’t be proud. Be alive.
Alex Piddington
December 10, 2025As someone who works in pain management, I can confirm: tolerance is a physiological reality, not a moral failing. The real tragedy isn’t the tolerance-it’s the lack of education around it. Patients deserve to know this before they’re stuck on escalating doses. We need mandatory patient education modules before long-term opioid prescriptions. It’s not just ethical-it’s lifesaving.
Pavan Kankala
December 10, 2025They say tolerance is biology. But who controls the science? Who funds the studies? Who owns the patents? The same corporations that sold us this crisis. Tolerance is a myth. It’s a distraction. The real problem is control. They want you dependent. They don’t want you cured. They want you paying. Always paying.