15 Dec 2025
- 14 Comments
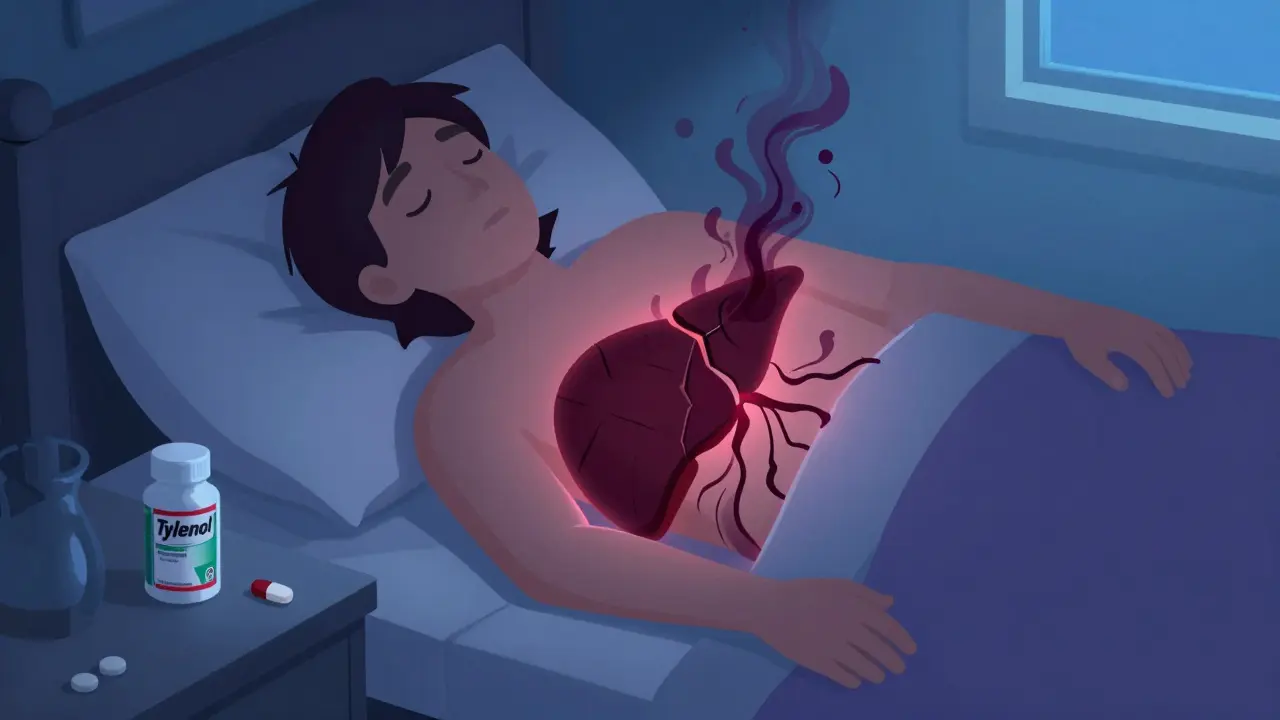
Every year, more than 56,000 people in the U.S. end up in the emergency room because they took too much acetaminophen. That’s more than any other drug overdose. And it’s not just street drugs or prescription abuse - it’s often someone who thought they were being careful. Maybe they took one extra pill for a headache. Or doubled up because the pain didn’t go away. Or didn’t realize their cold medicine already had it in there. The result? A silent, deadly attack on the liver - one that can start without symptoms and spiral into failure within hours.
What Happens When You Take Too Much Acetaminophen?
Acetaminophen, sold as Tylenol or paracetamol, is safe when used as directed. But your liver can only handle so much. The maximum safe dose for adults is 4,000 milligrams in 24 hours - that’s eight 500 mg pills. Go over that, and your liver starts to break down the drug into a toxic chemical called NAPQI. Normally, your body neutralizes it with glutathione, an antioxidant. But when you overdose, glutathione runs out. NAPQI then starts destroying liver cells. This isn’t a slow process. It happens fast. And you might not feel anything until it’s too late.
Stage 1: The Quiet Hours (0-24 Hours)
Right after an overdose, many people feel fine. Or maybe just a little nauseous. About 78% throw up. Around 65% lose their appetite. But 30 to 40%? They feel nothing at all. That’s the danger. No pain. No jaundice. No confusion. Just silence. People assume they’re okay. They go to bed. They wait it out. But inside, the liver is already under siege. By the time symptoms show up, the damage is often advanced.
Stage 2: The First Warning Signs (24-72 Hours)
This is when things start to turn serious. Right upper abdominal pain - the kind that feels deep and constant - hits 85% of people. Nausea and vomiting come back, stronger this time. Blood tests begin to show trouble: liver enzymes like ALT start climbing. Normal ALT? 7 to 56 IU/L. In overdose cases, it can jump to over 10,000. That’s a 200-fold increase. Your liver isn’t just stressed - it’s dying. If you’re here, you need treatment now.
Stage 3: The Crisis Point (72-96 Hours)
This is the peak. The liver is failing. Jaundice - yellow skin and eyes - appears in 92% of severe cases. Your blood can’t clot properly. Your INR (a clotting test) might be over 1.5, sometimes above 6.5. You might feel confused, drowsy, or even slip into a coma. Kidneys start to shut down. About half of people with full liver failure also develop kidney damage. Pancreatitis can kick in too. Without treatment, death is likely. But here’s the critical truth: if you get help before this stage, survival chances are above 90%.
Stage 4: Recovery or Death (Beyond 5 Days)
If you survive, your liver can heal - if it wasn’t too badly damaged. About 85 to 90% of people who get treated on time make a full recovery. Their liver regenerates. Blood tests return to normal. Within three months, 92% of survivors have no lasting damage. But if treatment is delayed, the mortality rate jumps from under 1% to over 25%. And if you’re in the worst group - with a blood pH below 7.3, INR over 6.5, and creatinine above 3.4 - your chance of surviving without a transplant is zero.
The Only Antidote: N-Acetylcysteine (NAC)
There’s one drug that can save you: N-acetylcysteine, or NAC. It works by replacing the glutathione your body used up and mopping up the toxic NAPQI. The sooner you get it, the better. If you’re treated within 8 hours of taking too much, NAC is 98% effective. After 15 hours, it drops to 55%. That’s why every minute counts.
The standard IV protocol is a 21-hour drip: 150 mg/kg over the first hour, then 50 mg/kg over the next four hours, then 100 mg/kg over the final 16 hours. Oral NAC takes longer - 72 hours - and is harder to keep down if you’re vomiting. But both work if given early enough. Even if you show up 24 hours later, NAC still helps. Doctors give it anyway - because it’s safer than not giving it.
What Else Do Doctors Do?
If you arrive within 1 to 2 hours of taking the overdose, they’ll give you activated charcoal. It traps the drug in your gut so it doesn’t get absorbed. They’ll also give you IV fluids to keep your kidneys working. Anti-nausea meds like ondansetron help you keep down the NAC. If your blood won’t clot, they’ll give you vitamin K or fresh frozen plasma. All of this supports your body while NAC does its job.
Who’s at Highest Risk?
It’s not just people who take pills intentionally. Many overdoses are accidental. Here’s who’s most vulnerable:
- Chronic drinkers: Alcohol makes your liver produce more of the toxic enzyme that turns acetaminophen into NAPQI. Risk goes up 3 to 4 times.
- People with hepatitis B or C: Their livers are already damaged. Acetaminophen hits them harder - up to 65% more risk.
- Those on seizure meds: Drugs like phenytoin or carbamazepine speed up the toxic pathway. Risk increases by 40%.
- People with poor nutrition: Low protein intake cuts glutathione by 25-30%. Fasting, eating disorders, or even long-term dieting can make you more sensitive.
And here’s the biggest hidden risk: combination painkillers. Vicodin, Percocet, Excedrin - they all contain acetaminophen. Someone might take two Vicodin for back pain, then grab two Tylenol for a fever. That’s 1,200 mg of acetaminophen in one go. Do that three times a day? You’re over the limit. And most people don’t know.
How Do Doctors Know If You Need NAC?
They use the Rumack-Matthew nomogram. It’s a graph that plots your blood acetaminophen level against time. If you come in 4 hours after taking the pills, they draw your blood. If the level is above 150 µg/mL, you get NAC. If it’s below? You’re probably safe. But if you’re not sure when you took it - or if you took multiple doses over time - they treat you anyway. Better safe than sorry.

What About Liver Transplants?
Only 1 to 2% of acetaminophen overdoses lead to liver failure severe enough to need a transplant. But when it does, it’s life or death. The King’s College Criteria help doctors decide: if you have a blood pH below 7.3, INR over 6.5, and creatinine above 3.4 mg/dL - you need a new liver. Without one, death is certain. With one? Eighty-five percent survive at least five years. That’s better than many cancer survival rates.
Why Is This Still Happening?
In 2011, the FDA forced drugmakers to lower the maximum acetaminophen dose in prescription pills from 750 mg to 500 mg. That cut liver failure cases by 21% over 11 years. But it’s not enough. People still don’t know how much is too much. They think, “It’s over-the-counter, so it’s harmless.” They don’t check labels. They combine meds. They ignore warnings. And by the time they feel sick, it’s often too late.
What You Can Do Right Now
- Never take more than 4,000 mg of acetaminophen in 24 hours - even if you’re in pain.
- Always check the labels of cold, flu, and pain meds. Many contain acetaminophen.
- If you drink alcohol regularly, limit acetaminophen to 2,000 mg a day - or avoid it altogether.
- If you have liver disease, talk to your doctor before taking any acetaminophen.
- If you think you’ve taken too much - even if you feel fine - go to the ER. Don’t wait.
The window to save your liver is narrow. Eight hours. That’s it. If you’re unsure, call poison control. Or head to the hospital. It’s not dramatic. It’s not scary. It’s just smart. And it could mean the difference between walking out on your own - or needing a transplant.
What’s Next in Treatment?
Scientists are looking at new ways to help. Early research at Harvard shows nitric oxide might boost liver regeneration - even after the 8-hour window. Another promising tool? MicroRNA-122, a blood marker that rises within two hours of overdose. It’s 94% accurate at spotting liver damage before symptoms appear. If it gets approved, we could have a simple blood test to catch overdoses before they become disasters.
For now, though, the best tool is awareness. Know the limits. Check the labels. Don’t assume. And if you’re ever in doubt - get help. Your liver doesn’t scream. It just stops working. Don’t wait for it to say something.
Can you survive an acetaminophen overdose without treatment?
Yes, but only if the overdose was very small and caught early. Most people who take more than 7,500 mg without treatment develop severe liver damage. Without NAC, the death rate jumps from under 1% to over 25%. Even if you feel fine, you can’t rely on symptoms - the damage is silent until it’s too late.
Is it safe to take acetaminophen every day?
For most healthy adults, taking 3,000 to 4,000 mg a day for a few days is okay. But daily use over weeks or months - even at 3,000 mg - can cause gradual liver damage, especially if you drink alcohol or have hepatitis. Doctors recommend the lowest effective dose for the shortest time. If you need pain relief daily, talk to your doctor about alternatives.
Can children overdose on acetaminophen too?
Yes. Children’s dosing is based on weight, not age. Giving a child a regular adult tablet can be deadly. Always use the measuring device that comes with the medicine. Never guess the dose. If you think your child took too much, call poison control immediately - even if they seem fine.
How long does it take for liver damage to show up after an overdose?
Liver enzyme levels start rising within 12 to 24 hours, but visible signs like jaundice or confusion usually appear between 72 and 96 hours. By then, the damage is often severe. That’s why early blood tests and NAC are critical - you can’t wait for symptoms to act.
Does NAC have side effects?
IV NAC can cause nausea, vomiting, flushing, or low blood pressure - especially if given too fast. But these are usually mild and manageable. The risk of not giving NAC is far greater. Oral NAC tastes awful and often causes vomiting, which is why IV is preferred in emergencies.
Can you take NAC as a supplement to prevent liver damage?
No. Over-the-counter NAC supplements are not proven to prevent acetaminophen overdose damage. They’re not regulated the same way as medical-grade NAC. Only the IV or oral protocol given in a hospital under medical supervision works to reverse overdose. Don’t rely on supplements for protection.
What should you do if you suspect someone overdosed on acetaminophen?
Call emergency services or go to the nearest ER immediately. Don’t wait for symptoms. Bring the medicine bottle with you so doctors know the strength and amount taken. If possible, note the time of ingestion. Even if they seem fine, treat it as a medical emergency. Every minute counts.

James Rayner
December 16, 2025Just read this at 3 a.m. after my headache got worse... and I realized I’ve been taking two Tylenol with my nightly whiskey for months. 😳 I’m not even mad at myself-I’m just... stunned. My liver didn’t scream. It just quietly started packing its bags.
Dan Padgett
December 18, 2025Man, this hit different. In Nigeria, folks think Tylenol is like water-no harm, no foul. But now I see: it’s not the pill that kills. It’s the silence after you take it. 🤕
Hadi Santoso
December 19, 2025So I just checked my medicine cabinet… and holy crap. Excedrin, NyQuil, Vicodin, and two bottles of ‘pain relief’ from the gas station-all with acetaminophen. I thought I was being smart by ‘rotating’ meds. Turns out I was just playing Russian roulette with my liver. 🤦♂️
Kayleigh Campbell
December 20, 2025So let me get this straight-my grandma’s ‘natural remedy’ for headaches is two Advil and a Tylenol because ‘they work better together’… and you’re telling me she’s one wrong dose away from needing a new liver? 😅
Joanna Ebizie
December 22, 2025People are idiots. You think because it’s OTC it’s safe? My cousin died from this. She didn’t even know her cold medicine had it. And now her kids have to grow up without her. Just… don’t be that person.
Elizabeth Bauman
December 22, 2025THIS is why we need stricter laws. In China, they put warning labels in 12 languages. In Canada, they limit pack sizes. But here? We let people kill themselves with candy-colored pills because ‘freedom.’ 🇺🇸
Kitty Price
December 24, 2025I’m gonna print this out and tape it to my medicine cabinet. 🙏
Colleen Bigelow
December 24, 2025Big Pharma knows this. They’ve known for decades. Why didn’t they change the labeling? Why didn’t they make the pills harder to overdose on? Because profit > people. And now we’re all paying the price.
Randolph Rickman
December 25, 2025I’m a nurse, and I’ve seen this too many times. People show up at 3 a.m. saying ‘I just took one extra pill.’ One extra pill. One extra pill. And now their liver’s a goner. Don’t be that person. If you’re unsure-go. Just go. NAC saves lives. And it’s free if you’re in the ER.
sue spark
December 26, 2025I’ve been taking 3000mg daily for my chronic back pain and never thought twice. I’m cutting it to 2000mg starting today. Thank you for this. I didn’t know I was playing with fire
SHAMSHEER SHAIKH
December 27, 2025Esteemed colleagues, I have observed with profound concern the alarming prevalence of acetaminophen-related hepatotoxicity in Western nations. The absence of public health literacy in pharmacological dosing constitutes a systemic failure of medical education and regulatory oversight. It is imperative that we institute mandatory labeling protocols, similar to those in India, wherein every tablet bears a bold, multilingual warning: 'DO NOT EXCEED 4000 MG IN 24 HOURS - LIVER FAILURE MAY OCCUR WITHOUT SYMPTOMS.'
Souhardya Paul
December 29, 2025My mom used to say ‘if a little helps, more must be better.’ I didn’t realize she was teaching me how to kill myself slowly. I’m gonna start keeping a log now. And I’m gonna make my whole family read this.
Josias Ariel Mahlangu
December 30, 2025You people are too soft. If you can’t handle a little pain, you shouldn’t be taking pills. Just toughen up. This isn’t a tragedy-it’s a lesson. And you didn’t learn it.
anthony epps
December 31, 2025Wait so if I took 2 Tylenol at 8am and then 2 more at 10pm, that’s 1000mg. Then I take a cold med with 325mg at midnight? That’s still under 4000 right? Or am I missing something?