20 Jan 2026
- 11 Comments
Have you ever taken a pill with your breakfast and wondered why it didn’t seem to work as well as it should? Or maybe you skipped a dose because you weren’t sure whether to take it before or after eating. You’re not alone. Many people don’t realize that what’s on their plate can make or break how well their medicine works.
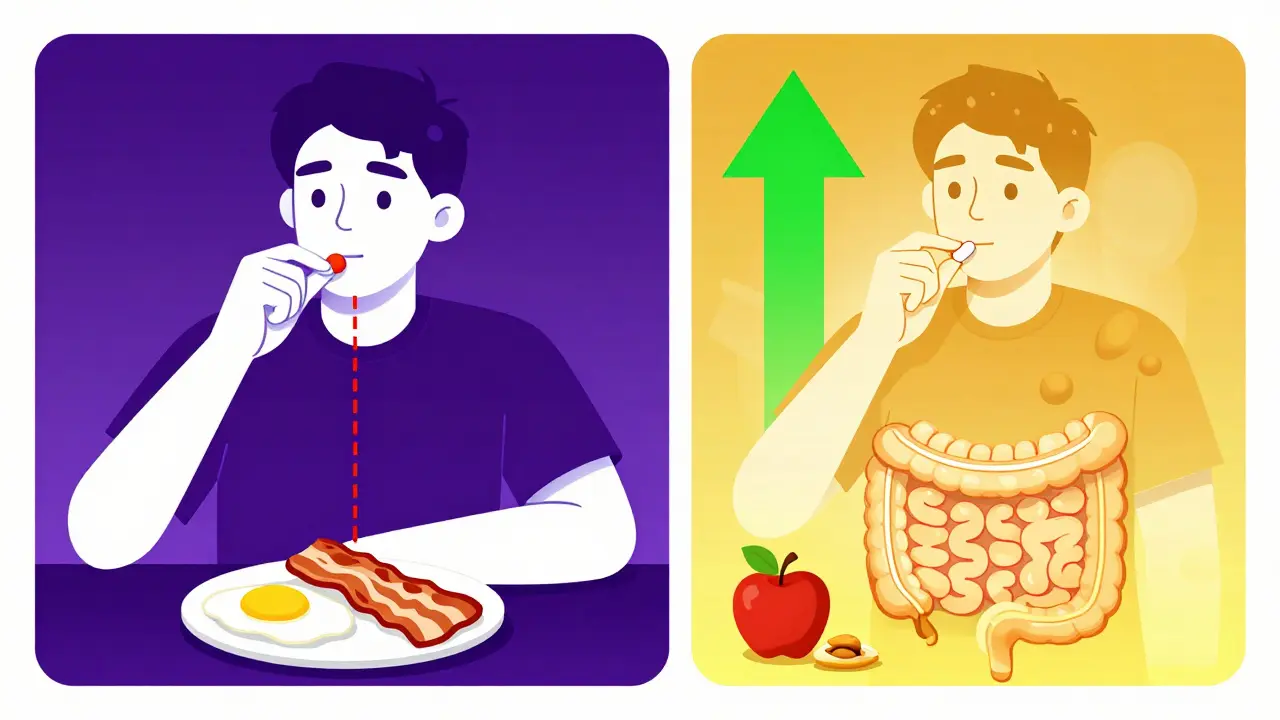
The truth is, food doesn’t just fill your stomach - it changes how your body handles medicine. Some drugs work better when taken with food. Others can become useless - or even dangerous - if eaten at the same time. Getting this wrong isn’t just inconvenient. It can lead to treatment failure, side effects, or hospital visits.
Why Food Changes How Medicines Work
Your digestive system doesn’t treat every pill the same way. When you eat, your stomach slows down. Gastric emptying - the process that moves food and pills into your small intestine - can take 30% to 50% longer after a meal. That delay changes when the medicine gets absorbed.
Some medications need that delay. Others need speed. Fats in food can help dissolve certain drugs, making them easier to absorb. Calcium in dairy can block others. Acid levels in your stomach drop after eating, which can stop some pills from breaking down properly.
These aren’t random effects. They’re predictable, well-studied, and documented. The FDA requires drug makers to test how food affects their products. If a pill’s absorption changes by more than 20% with food, it has to say so on the label.
Medications That Need an Empty Stomach
Some drugs are like delicate plants - they only thrive in clean soil. Take levothyroxine, the most common thyroid hormone replacement. Food, especially calcium, iron, or soy, can cut its absorption by 30% to 55%. That means your body doesn’t get enough hormone, and your fatigue, weight gain, or depression won’t improve - even if you’re taking the right dose.
Experts recommend taking levothyroxine at least 30 to 60 minutes before breakfast, with plain water only. No coffee, no orange juice, no toast. Just wait.
Same goes for tetracycline and doxycycline, antibiotics often used for acne or infections. Calcium in milk, yogurt, or antacids binds to these drugs and traps them in your gut. One Reddit user shared how a recurring UTI didn’t clear up until they stopped taking doxycycline with their morning yogurt. Two hours apart - that’s all it took.
Other medications that need an empty stomach:
- Bisphosphonates (like alendronate for osteoporosis) - must be taken with plain water on an empty stomach, and you must stay upright for 30 minutes after.
- Some antifungals (like itraconazole) - need stomach acid to work. Food raises pH and lowers absorption by up to 40%.
- Semaglutide (Ozempic, Wegovy) - absorption drops 44% if taken within 30 minutes of eating.
Medications That Work Better with Food
Not all pills hate food. Some actually need it.
Nitrofurantoin, a common UTI antibiotic, absorbs 40% better when taken with food. The same goes for cefpodoxime, another antibiotic - food boosts absorption by 50% to 60%.
Then there’s griseofulvin, an old-school antifungal for nail infections. With a high-fat meal, your body absorbs 200% to 300% more of it. That’s not a small boost - it’s the difference between treatment working and failing.
Even some painkillers benefit. NSAIDs like ibuprofen and naproxen can irritate your stomach lining. Taking them with food reduces the risk of ulcers and acid reflux. A GoodRx survey found stomach pain dropped from 42% to 12% when people took ibuprofen with meals.
Other medications that work better with food:
- Sulfonylureas (glipizide, glyburide) - diabetes drugs that can cause dangerous low blood sugar if taken without food. Taking them 30 minutes before a meal helps match insulin release with food intake.
- Atazanavir (an HIV drug) - requires food to reach effective levels in the blood.
- Statins like simvastatin - absorption improves slightly with food, though timing is less critical than for other drugs.
What Does “With Food” Really Mean?
Here’s where confusion sets in. When a label says “take with food,” does that mean a full meal? A snack? A handful of almonds?
According to the Australian Prescriber and FDA guidelines, “with food” means taking the pill within 30 minutes of starting your meal. It doesn’t have to be a big meal. For many drugs, even a small snack of 200-300 calories is enough.
But here’s the catch: not all snacks are equal. A banana and peanut butter? Fine. A protein bar with calcium? Might interfere. A glass of milk with your antibiotic? Bad idea.
One of the biggest mistakes patients make? Assuming “with food” means “with a big breakfast.” In reality, for drugs like certain antiretrovirals or HIV meds, a light snack is all you need. Too much fat or calcium can backfire.
Pharmacists see this all the time. A 2022 study found that 45% of patients misunderstood “take with food.” Thirty-two percent thought they needed a full meal - and took their pill with a heavy breakfast, which actually reduced absorption for some drugs.
Timing Matters More Than You Think
It’s not just whether you take your pill with food - it’s when.
For example, glipizide, a diabetes pill, is designed to trigger insulin release 30 minutes after you eat. If you take it on an empty stomach, your blood sugar can crash. The American Diabetes Association reports that 23% of patients on sulfonylureas who skip meals end up with symptoms of low blood sugar - shaking, sweating, confusion - and need emergency help.
On the flip side, taking levothyroxine right after breakfast? Absorption drops. Taking it at night? Some studies show it works just as well - if your stomach is truly empty. But most doctors still recommend morning dosing because it’s easier to stick to.
Even something as simple as coffee can interfere. Caffeine can speed up gastric emptying, which might cause some drugs to hit your system too fast. For others, it can reduce absorption. The rule? Stick to water for 30 to 60 minutes before and after your pill.
Who’s Most at Risk?
Not everyone is equally likely to mess this up.
Older adults on five or more medications - what doctors call polypharmacy - have a 65% higher risk of food-drug interactions. They’re juggling pills for blood pressure, diabetes, arthritis, and heart disease. One wrong timing decision can ripple across their whole treatment plan.
People with chronic conditions like thyroid disease, HIV, or diabetes are especially vulnerable. Their meds are finely tuned. A 20% drop in absorption can mean the difference between control and crisis.
And let’s not forget cost. The U.S. spends over $500 billion a year on medication-related problems. Food-drug interactions contribute to about 8% of that - roughly $40 billion. That’s not just a health issue. It’s an economic one.

How to Get It Right
You don’t need to memorize every drug interaction. But you can take simple steps to protect yourself.
- Read the label. Look for phrases like “take on an empty stomach,” “take with food,” or “avoid dairy.”
- Ask your pharmacist. They’re trained to catch these details. Don’t assume your doctor explained it. Pharmacists see hundreds of patients a week - they know what trips people up.
- Use a pill organizer with reminders. Apps like Medisafe and MyTherapy let you set food-based alerts: “Take with breakfast,” “Wait 60 minutes after eating.” Users who turn these on have 27% fewer timing errors.
- Be consistent. If you take your pill with food, always take it with food. If you take it on an empty stomach, always do it the same way. Inconsistency is what causes therapeutic failure.
- Keep a log. Note what you ate and when you took your pill. If you feel off, you’ll have a record to show your doctor.
And if you’re ever unsure? Wait. Don’t guess. Call your pharmacy. Or wait until you can eat - better safe than sorry.
The Future of Food and Medicine Timing
This isn’t just about old rules. New tech is changing the game.
Researchers are now testing ingestible sensors that track stomach pH and emptying speed in real time. One 2023 trial showed that patients using these sensors improved drug absorption by 38% for pH-sensitive drugs.
And it’s not just about food anymore. Scientists are studying when you take your pill - not just with food, but at what time of day. Circadian rhythms affect how your body absorbs and processes drugs. A 2024 study in Nature Medicine found that timing certain heart and diabetes meds to your body’s natural clock improved results by up to 30%.
Meanwhile, the FDA is updating its guidelines to reflect modern diets. The old standard high-fat meal? It’s being replaced with plant-based, gluten-free, and low-sugar options to match what people actually eat today.
One thing’s clear: the days of “take with food” as a vague instruction are over. Precision matters.
Bottom Line: Don’t Guess. Know.
Your medicine is powerful. But it’s not magic. It needs the right environment to work. Food isn’t just fuel - it’s part of your treatment plan.
For some pills, food helps. For others, it blocks. Timing can make the difference between healing and harm.
Don’t rely on memory. Don’t assume you know. Check the label. Ask your pharmacist. Set a reminder. Your body - and your health - will thank you.


Uju Megafu
January 20, 2026OMG I CAN’T BELIEVE PEOPLE STILL TAKE LEVOTHYROXINE WITH COFFEE. I HAD A FRIEND WHO WAS ON IT FOR 5 YEARS AND HER TSH WAS ALWAYS CRAZY BECAUSE SHE DRANK HER MORNING LATTE 10 MINUTES AFTER HER PILLS. SHE THOUGHT IT WAS ‘FINE’ UNTIL HER ENDOCRINOLOGIST CALLED HER OUT. NOW SHE TAKES IT AT NIGHT WITH WATER AND SLEEPS LIKE A BABY. WHY IS THIS EVEN A QUESTION???
MAHENDRA MEGHWAL
January 21, 2026Thank you for this comprehensive and meticulously researched exposition. The pharmacokinetic principles elucidated herein are of profound clinical significance, particularly in resource-constrained settings where patient education is often inadequate. I shall ensure that this information is disseminated within my professional network.
Kevin Narvaes
January 22, 2026so like… food is just… a vibe? like if you’re vibin’ with your breakfast, your pills are like ‘oh cool, i’ll absorb now’? but if you’re stressed about toast? they just sit there like ‘nah i’m out’??
also why is everyone so mad about dairy? i just drink almond milk now and i’m fine??
also i think god made coffee to help meds work better idk
Dee Monroe
January 23, 2026It’s fascinating how deeply our bodies are wired to respond not just to what we consume, but when and how we consume it. We’ve been conditioned to think of medicine as a magic bullet - pop a pill, fix the problem - but the truth is, our digestive system is an entire symphony of chemistry, timing, and environment. When we ignore the rhythm of our meals, we’re essentially conducting that symphony with a broken baton. Levothyroxine isn’t just a hormone replacement - it’s a signal to your entire endocrine orchestra. And if you’re eating soy yogurt while it’s trying to sing? The whole piece collapses. We treat our bodies like machines, but they’re living, breathing ecosystems - and food isn’t just fuel, it’s the language they speak.
Rod Wheatley
January 24, 2026YES! YES! YES! I’m a nurse, and I’ve seen so many people mess this up - especially seniors on 8+ meds. I always tell them: ‘If it says ‘empty stomach,’ don’t even think about your coffee, your toast, your banana, your probiotic yogurt, or your dog’s breath.’ Just water. Just wait. Just do it. And if you forget? Don’t double up - wait until tomorrow. Your body doesn’t care if you ‘forgot’ - it just knows you messed up the timing. Use apps. Set alarms. Write it on your fridge. This isn’t optional - it’s survival. You’re not being ‘annoying’ - you’re being smart.
Jerry Rodrigues
January 26, 2026Good post. I take atazanavir with a peanut butter sandwich every night. Never had an issue. I used to take it on an empty stomach because I thought that’s what ‘best’ meant. Turned out I was making it harder on myself. Food isn’t the enemy. Misinformation is.
Yuri Hyuga
January 26, 2026This is GOLD 🙌 I’ve been telling my clients for years: ‘Take your meds like you’re tucking your body in for bed - with care, consistency, and zero distractions.’ Food isn’t just nutrition - it’s your medicine’s co-pilot. And if you’re not training your co-pilot? You’re flying blind. 💡
P.S. If you’re on statins, don’t eat grapefruit. I know, I know - it’s delicious. But your liver is not a fan. 🍊🚫
MARILYN ONEILL
January 27, 2026So basically, if you’re not rich enough to afford a nutritionist, you’re just supposed to guess? And if you take your pill wrong? Too bad. Your body’s just supposed to suffer? This is why people hate doctors. You give us a list of rules and no one explains why. And then you blame us for not reading the tiny print on the bottle that’s written in font size 4.
Coral Bosley
January 28, 2026I’ve been taking my antibiotics with pizza for 3 years and I’m still alive. You people are so scared of food. It’s not a poison. It’s just… food. You think your body can’t handle it? You’re the one who’s broken, not the medicine.
shubham rathee
January 29, 2026i think this whole food and meds thing is a big pharma scam to sell more pills and apps like medisafe. if your body is healthy you dont need to time pills like a rocket launch. i take my stuff whenever i remember and i feel fine. also why are you all so scared of calcium? its just milk. its natural. the body knows what to do. stop overthinking. just live.
Alex Carletti Gouvea
January 30, 2026Look, I’m not some science bro, but I’ve been on 7 different meds since I got back from Iraq. I take them with my coffee, with my protein shake, with my burrito - and I’m still standing. If your body can’t handle real American food, maybe you shouldn’t be on meds at all. This country’s got bigger problems than whether you took your pill with yogurt.