21 Dec 2025
- 10 Comments
When you’re diagnosed with heart failure, especially with reduced ejection fraction (HFrEF), the right medications can mean the difference between struggling to breathe and living well. Four drug classes form the backbone of modern treatment: ACE inhibitors, ARNI, beta blockers, and diuretics. These aren’t just pills - they’re tools that rewrite how your heart and blood vessels work. And the science behind them has changed dramatically in the last decade.
ACE Inhibitors: The Original Game Changer
ACE inhibitors were the first major breakthrough in heart failure treatment. Captopril hit the market in 1981, and by the late 1980s, studies like the CONSENSUS trial showed enalapril cut death rates by 27% in severe heart failure. These drugs block the enzyme that turns angiotensin I into angiotensin II - a powerful blood vessel constrictor. Less angiotensin II means lower blood pressure, less strain on the heart, and slower damage to heart muscle.Common ACEIs include lisinopril, enalapril, and ramipril. Dosing starts low - often 2.5 to 5 mg daily - and slowly increases over weeks. Target doses? For lisinopril, it’s 20-40 mg daily; for enalapril, 10-20 mg twice daily. But getting there isn’t easy for everyone.
The biggest side effect? A dry, persistent cough. It hits 5-20% of users and can be so annoying people stop taking the drug. Others face high potassium levels (hyperkalemia), which can be dangerous if not caught early. Rarely, swelling of the face or throat (angioedema) occurs - a medical emergency. Still, for years, ACEIs were the gold standard. Now, they’re being replaced - but only if you can tolerate them.
ARNI: The New First-Line Standard
In 2015, everything shifted. The FDA approved sacubitril/valsartan (brand name Entresto), the first ARNI. Unlike ACEIs or ARBs, ARNIs do two things at once: they block angiotensin receptors (like ARBs) and boost natriuretic peptides (like natural heart hormones that help flush out salt and water). This dual action reduces heart strain more effectively than ACEIs alone.The PARADIGM-HF trial, which followed nearly 8,400 patients across 47 countries, showed ARNI cut cardiovascular death and hospitalizations by 20% compared to enalapril. That’s not a small win - it’s a landmark. Today, the 2022 AHA/ACC/HFSA guidelines say ARNI should be the first choice for HFrEF patients who can tolerate it.
Starting dose is 24/26 mg twice daily, doubled every 2-4 weeks until you hit 97/103 mg twice daily. But here’s the catch: you can’t start ARNI within 36 hours of taking an ACEI. The risk of angioedema spikes. If you’re on lisinopril and your doctor switches you to Entresto, they’ll make you wait. That’s not a suggestion - it’s a safety rule.
Cost is a real barrier. Without insurance, Entresto runs about $550 a month. Generic ACEIs? As low as $4. That’s why only 42% of community clinics use ARNI as first-line, even though academic centers hit 65%. Insurance often requires prior authorization. But for patients who can access it, the payoff is clear. One Reddit user reported reduced shortness of breath within two weeks. That’s the kind of change that matters.
Beta Blockers: Slowing Down to Save the Heart
It sounds backwards - why slow down a heart that’s already struggling? But in heart failure, the body’s stress response goes into overdrive. The heart beats faster, pumps harder, burns energy it doesn’t have. Beta blockers calm that storm.Not all beta blockers work here. Only three are proven: carvedilol, metoprolol succinate, and bisoprolol. These are different from the ones used for high blood pressure or anxiety. They’re specially formulated for heart failure.
Carvedilol starts at 3.125 mg twice daily. Metoprolol succinate at 12.5 mg daily. Bisoprolol at 1.25 mg daily. All are increased slowly - every 2-4 weeks - only if your heart rate stays above 50 and you’re not getting worse. This isn’t a fast process. It can take months to reach target doses.
Why go through this? The CIBIS-II trial showed bisoprolol cut death by 34%. The COPERNICUS trial found carvedilol reduced mortality by 35%. One patient on Reddit saw their ejection fraction climb from 25% to 45% over 18 months. That’s not magic - it’s science.
Side effects? Fatigue, low blood pressure, dizziness, and slow heart rate. About 72% of users on PatientsLikeMe reported fatigue so bad they struggled to stick with the dose. But here’s the twist: those who stayed on it, even at lower doses, lived longer. It’s not about feeling great right away. It’s about surviving tomorrow.

Diuretics: Managing the Fluid, Not the Disease
Diuretics don’t fix heart failure. They don’t extend life. But they make you feel better - fast.When your heart fails, fluid backs up. Lungs fill. Ankles swell. Breathing gets hard. Diuretics flush that out. Loop diuretics like furosemide, bumetanide, and torsemide are the go-to. Furosemide starts at 20-80 mg daily. Torsemide? Often more effective - the EVEREST trial showed 18% fewer hospitalizations than furosemide.
Thiazides like hydrochlorothiazide are used for milder cases or added on. Spironolactone is special - it’s a diuretic and a mineralocorticoid receptor antagonist (MRA). The RALES trial proved it cut death by 30%. But it also raises potassium. That’s why doctors monitor blood levels closely.
Patients hate the side effects. Frequent urination. Nighttime bathroom trips. Leg cramps. One Reddit user said furosemide caused severe cramps until they started taking potassium and magnesium. Another said they couldn’t leave the house without planning for a bathroom. But here’s the truth: without diuretics, many patients wouldn’t be able to walk across the room. They’re the symptom relievers - the ones that let you breathe again.
The Big Picture: Quadruple Therapy and Why Most Patients Don’t Get It
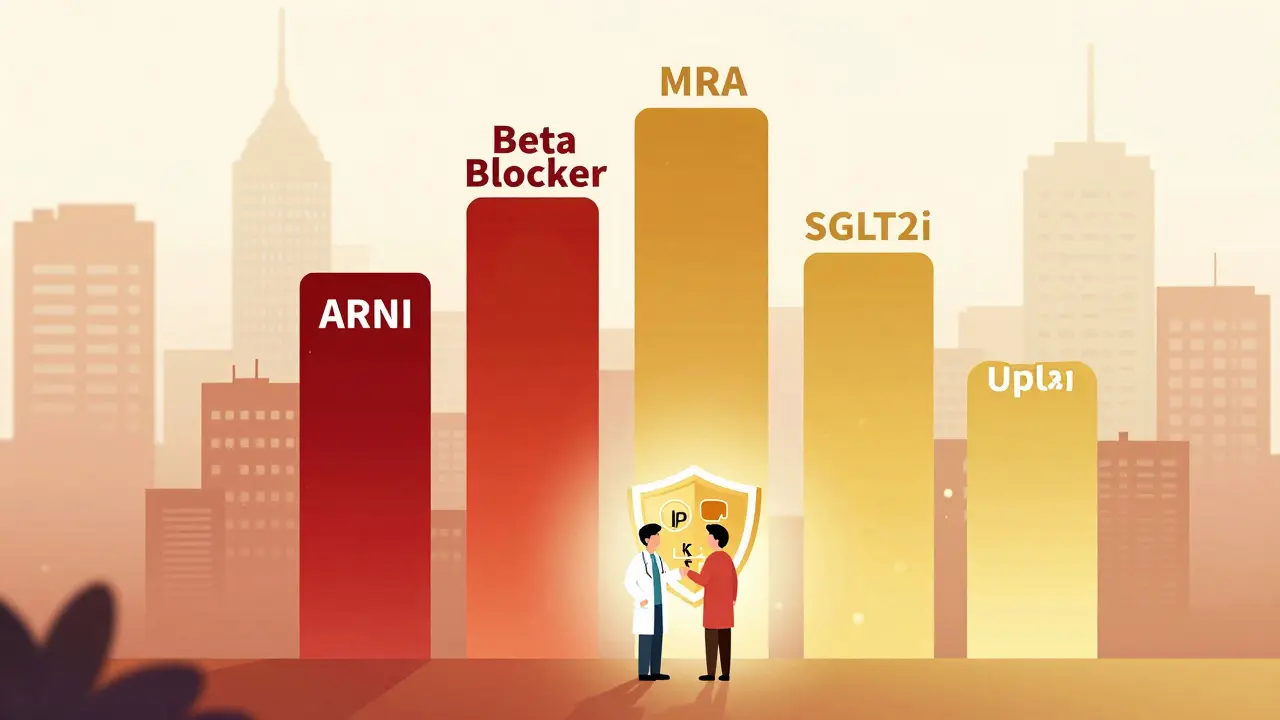
The ideal treatment today isn’t one or two drugs. It’s four: ARNI (or ACEI/ARB), beta blocker, MRA (like spironolactone), and SGLT2 inhibitor (like dapagliflozin). Diuretics are added as needed.Studies show this combination reduces death by up to 20% and hospitalizations by 21%. Yet, only 35% of eligible patients get all four within a year of diagnosis. Why?
First, titration is slow. Doctors fear low blood pressure or kidney issues. Patients fear side effects. Second, cost. ARNI and SGLT2 inhibitors are expensive. Third, access. Rural clinics don’t have heart failure specialists. A 2023 study found only 28% of eligible patients in underserved areas get guideline-recommended care.
Monitoring is key. Blood potassium, creatinine, and blood pressure must be checked within 1-2 weeks of starting or changing any of these drugs. Ejection fraction should be rechecked at 3-6 months. If your doctor isn’t tracking these, ask why.
What Patients Are Really Saying
Real-world experiences tell a different story than clinical trials.On PatientsLikeMe, 68% of users said they couldn’t tolerate target beta-blocker doses because of fatigue. 45% quit ACEIs because of the cough. But 82% of those on ARNI kept taking it - even though 58% felt dizzy at first - because they could finally walk without gasping.
Amazon reviews show ARNI has the highest rating (4.3/5) for effectiveness, but the biggest complaint is cost. Diuretics get high marks for symptom relief, but users hate the bathroom trips. Beta blockers? Valued for long-term survival, hated for exhaustion.
One user wrote: “I thought I was done. Then I switched to Entresto. Two weeks later, I carried my own groceries.” That’s the power of the right combination.
What’s Next?
The future is expanding. ARNI is now approved for heart failure with mildly reduced ejection fraction (HFmrEF), adding millions more eligible patients. SGLT2 inhibitors - originally for diabetes - are now recommended across all types of heart failure. New drugs like vericiguat are being added to the mix.But the biggest challenge isn’t new science. It’s getting the science to the people. Too many patients are still on outdated regimens. Too many doctors don’t titrate aggressively enough. Too many can’t afford the best options.
Heart failure isn’t a death sentence anymore. But it demands more than a prescription. It demands persistence, monitoring, and the courage to push through side effects - because the alternative is worse.
Can I take an ACE inhibitor and ARNI together?
No. Taking an ACE inhibitor and ARNI together within 36 hours increases the risk of angioedema - a dangerous swelling of the face, lips, or throat. If switching from an ACEI to ARNI, you must wait at least 36 hours. Always follow your doctor’s exact instructions on timing.
Why do beta blockers make me so tired?
Beta blockers slow your heart rate and reduce the force of each beat, which lowers your body’s energy use. That’s good for your heart long-term, but it can cause fatigue, dizziness, and low energy - especially when you first start or increase the dose. Most patients adjust over weeks or months. If fatigue is severe, talk to your doctor - your dose may need to be lowered temporarily.
Are diuretics dangerous?
Diuretics are generally safe when monitored. The main risks are dehydration, low potassium, low sodium, and kidney stress. Loop diuretics like furosemide can cause leg cramps or dizziness. Your doctor will check your blood levels regularly. Taking potassium or magnesium supplements (if recommended) can help. Never stop diuretics suddenly - fluid can build up fast.
Is ARNI better than ACE inhibitors?
Yes, for most patients with HFrEF. The PARADIGM-HF trial showed ARNI reduced death and hospitalizations by 20% compared to enalapril. ARNI also improves symptoms and quality of life more. If you can tolerate it and afford it, ARNI should replace ACEI as first-line therapy. But ACEIs still work well for those who can’t use ARNI.
How long does it take for these medications to work?
Diuretics work within hours - you’ll notice less swelling and easier breathing quickly. Beta blockers and ARNI take weeks to months. You won’t feel better right away, but your heart is healing. Blood pressure and heart rate may drop slowly. Ejection fraction improvements often show up after 3-6 months. Patience and consistency matter more than speed.
Can I stop these medications if I feel better?
No. Heart failure is a chronic condition. These medications don’t cure it - they manage it. Stopping them, even if you feel fine, can cause rapid worsening, hospitalization, or death. Always talk to your doctor before making any changes. Feeling better is a sign the drugs are working - not that you no longer need them.


Tony Du bled
December 22, 2025Just switched to Entresto last month. Two weeks in, I walked to the store without stopping to catch my breath. No joke. My wife cried. The cost is insane, but if you can get it, do it.
Kathryn Weymouth
December 24, 2025Important to note: the 36-hour washout period between ACEIs and ARNI isn't just a suggestion-it's a hard safety cutoff. I've seen patients admitted for angioedema because they skipped the waiting period. Always follow the protocol.
Art Van Gelder
December 25, 2025Let me tell you about my uncle-he was on lisinopril for years, coughing like he had a permanent cold. Then they switched him to ARNI. No more cough. No more wheezing at night. He started gardening again. But here’s the kicker: his insurance denied it for six months. He had to pay $500 out of pocket just to try it. When he finally got it, he said it felt like someone turned the volume down on his lungs. That’s not medicine-that’s magic with a prescription label.
And don’t get me started on beta blockers. I was on carvedilol for a year. Felt like a zombie. Couldn’t even walk the dog without needing a nap. But my EF went from 28% to 41%. So yeah, I’m tired. But I’m alive. And that’s the trade-off nobody talks about.
Diuretics? Oh man. I used to joke that my bladder had its own GPS. But without them, I’d be swollen like a balloon. One night, I had to pee so bad I did it in a coffee mug while standing in the kitchen. No shame. That’s heart failure. You adapt. You learn to live with the inconveniences. The alternative? You don’t get to joke about it at all.
And SGLT2 inhibitors? I didn’t even know they existed until my cardiologist mentioned them. ‘Wait, a diabetes drug helps my heart?’ Yeah. Turns out, your heart doesn’t care if you’re diabetic or not-it just wants to stop drowning in fluid and stress. It’s wild how science keeps rewriting the rules.
People think heart failure means you’re done. Nah. It means you’ve got to be smarter than your own body now. You’ve got to track potassium, time your meds, fight insurance, and still show up for life. It’s exhausting. But you can still live. Just… differently.
And if your doctor doesn’t check your labs within two weeks of changing a med? Find a new doctor. Seriously. This isn’t 2005 anymore. We’ve got data. We’ve got trials. We’ve got tools. Use them.
Johnnie R. Bailey
December 26, 2025As a nurse who’s worked in heart failure clinics for 18 years, I’ve watched this entire paradigm shift happen. I remember when ACEIs were the only game in town. Then beta blockers were ‘too risky.’ Now we’re talking about quadruple therapy as standard. The biggest barrier? Not the science-it’s the system. Rural clinics don’t have pharmacists who know how to titrate these meds. Patients get scripts and no follow-up. That’s why compliance plummets.
And cost? ARNI is $550/month. SGLT2 inhibitors? $400. Meanwhile, furosemide is $3. No wonder only 35% get the full regimen. Insurance prior auth forms are longer than the patient’s medical history. I’ve seen people skip doses because they can’t afford to refill. That’s not treatment-it’s triage.
But here’s what I tell every patient: You’re not just taking pills. You’re participating in your survival. The meds are tools. The real work? Showing up. Monitoring. Asking questions. Pushing back when you’re not heard. That’s the invisible therapy.
Cara Hritz
December 27, 2025Wait so ARNI is better then ACEI? I thought ACEI was the gold standard? My doc just put me on lisinopril and now im confused. Also why do i need 4 meds? I already take 8 pills a day. This is so much.
Jim Brown
December 29, 2025The evolution of heart failure pharmacotherapy is a profound illustration of the dialectical progression of medical science: from the crude but revolutionary inhibition of the renin-angiotensin axis, to the elegant dual modulation of neurohormonal pathways afforded by ARNI, and now the emergent recognition that metabolic modulation via SGLT2 inhibition confers cardiac benefit independent of glycemic control. The paradigm has shifted from palliation to regeneration, from symptom suppression to structural repair.
Yet, the chasm between evidence and access remains a moral indictment of our healthcare architecture. The fact that a patient’s prognosis hinges not on clinical need but on insurance formularies, geographic location, and socioeconomic status, betrays a fundamental dissonance between our professed values and our systemic practices.
One might argue that the human body, in its frailty, is the most honest critic of our institutions. When a man in rural Mississippi cannot afford Entresto while a man in Boston receives it without hesitation, we are not merely witnessing a disparity in pharmaceutical access-we are witnessing a fracture in the moral fabric of care.
Let us not mistake pharmacology for justice. The pills work. But the system? It still fails.
Jamison Kissh
December 30, 2025One thing nobody talks about: the psychological toll of chronic titration. You’re on a beta blocker. You feel like crap for three months. Your doctor says, ‘Just wait, it’ll get better.’ You wait. You keep taking it. You don’t know if it’s working. You don’t feel different. Then one day, your echo shows EF up 15 points. You didn’t feel that change. You just endured it. That’s the silent contract of heart failure meds-you trade present misery for future survival. And you do it alone.
It’s not just physical. It’s existential. You’re not just managing a disease. You’re negotiating with time.
Sam Black
December 31, 2025Been on all four pillars for 14 months now. The diuretics? Still hate them. But I carry a little water bottle with me now. No more ‘emergency bathroom’ panic. The ARNI? I get dizzy sometimes, but I can play with my grandkids without stopping. Beta blockers? Still tired. But I sleep better now. The real win? I haven’t been hospitalized since I started this combo. That’s not luck. That’s science. And it’s worth every side effect.
To anyone scared to start: I was too. But I’m still here. And I’m walking. That’s enough.
Aliyu Sani
December 31, 2025Yo i been on this stuff for a year and i think the real problem is the doctors dont tell you how to take it right. Like i took my ARNI with food and i got real dizzy. Then i found out you gotta take it on empty. Also why do they give you spironolactone if it makes your nuts shrink? I mean like… why? I’m not even joking. My bro said his girlfriend lost her boobs on it. That’s wild.
But hey, i can walk to the store now. So i guess it works. Just wish someone told me the side effects before i started.
Sai Keerthan Reddy Proddatoori
January 1, 2026They want you to take all these pills because Big Pharma owns the FDA. ACE inhibitors worked fine for 30 years. Now they say ARNI is better? Maybe because it costs 100x more. Diuretics make you pee too much? That’s because they want you to buy more diapers. Beta blockers make you tired? So you’ll buy more coffee. This is all a scam. The real cure is fasting and sunlight. But they won’t tell you that.