19 Nov 2025
- 8 Comments
Renal Dosing Calculator for Elderly Patients
Medication Dosing Calculator
Calculate your creatinine clearance (CrCl) and get dosing recommendations for medications that require adjustment based on kidney function.
Your Results
When you’re over 65 and your kidneys aren’t working like they used to, even a normal dose of a common pill can become dangerous. It’s not about being old-it’s about how your body changes. Kidneys filter drugs out of your blood. When they slow down, those drugs build up. And that buildup can cause falls, confusion, hospital stays, or even death. This isn’t rare. Nearly 4 in 10 adults over 65 have kidney damage severe enough to change how their meds work.
Why Kidney Function Matters More After 65
Your kidneys don’t just remove waste. They clear out most of the medications you take. As you age, kidney function drops naturally-even if you’re healthy. The glomerular filtration rate (GFR), which measures how well your kidneys filter blood, declines by about 1% per year after age 40. By 70, it’s often half what it was at 30. But here’s the catch: doctors still prescribe the same doses they’d give a 40-year-old. That’s because many rely on serum creatinine alone-a blood test that’s misleading in older people. Creatinine levels stay low even when kidneys are failing, because older adults have less muscle mass. So a "normal" creatinine reading can hide serious kidney damage. The real problem? Medications like digoxin, lithium, gabapentin, and certain antibiotics stick around much longer in elderly bodies. For example, digoxin’s safe range is tiny: 0.8 to 2.0 ng/mL. Go just a little over, and you risk fatal heart rhythms. Many patients never get their levels checked. And that’s just one drug.How to Measure Kidney Function Accurately
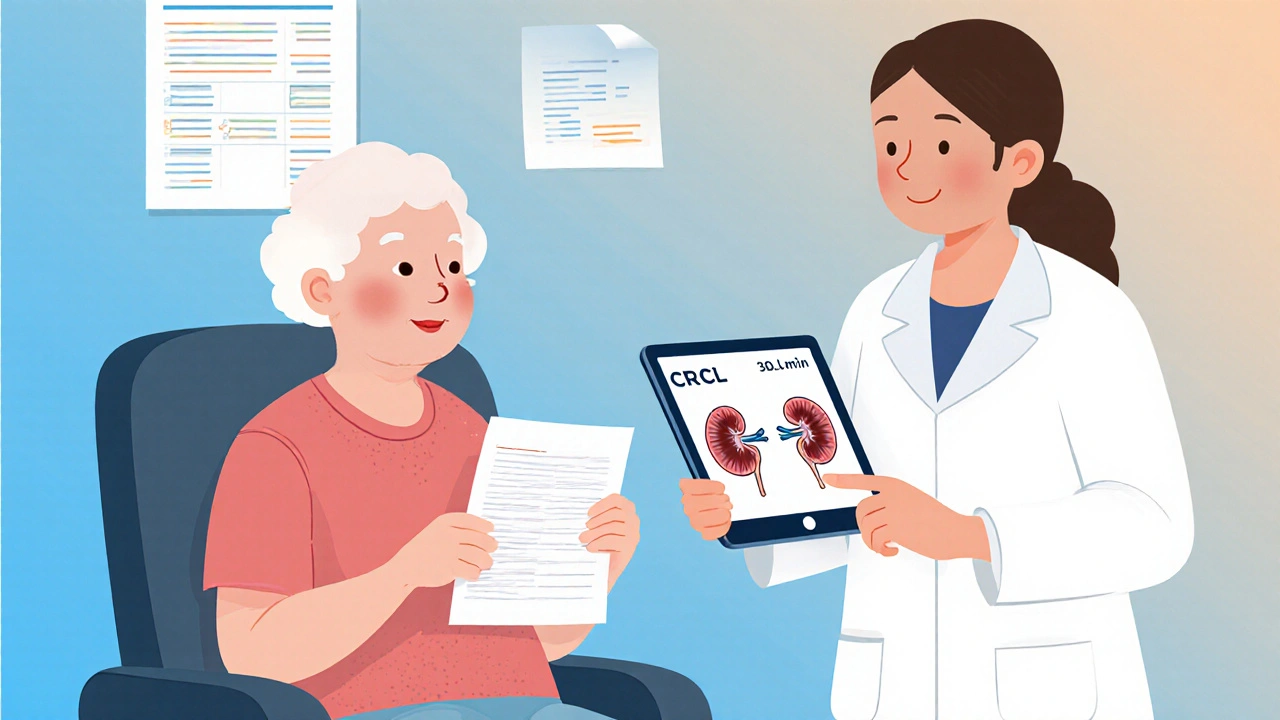
You can’t just look at a creatinine number. You need to calculate how well your kidneys are actually working. Two equations are used most often: Cockcroft-Gault and MDRD. The Cockcroft-Gault equation estimates creatinine clearance (CrCl) using your age, weight, sex, and serum creatinine. It’s older, but still preferred for dosing in elderly patients because it’s more conservative. The formula looks like this:CrCl = [(140 − age) × weight (kg)] ÷ (72 × serum creatinine) × 0.85 (if female)
For example, a 78-year-old woman weighing 60 kg with a creatinine of 1.2 mg/dL would have a CrCl of about 38 mL/min. That’s below the 50 mL/min threshold where many drugs need adjustment.
The MDRD equation estimates GFR and is more accurate for people with normal or mildly reduced kidney function. But in elderly patients, it often overestimates kidney function by 15-20%, which can lead to dangerous under-dosing. That’s why KDIGO guidelines recommend using Cockcroft-Gault for dosing decisions in older adults, especially when CrCl is near the critical 30 mL/min cutoff.
For even better accuracy, newer tests use cystatin C-a protein that’s less affected by muscle mass. The 2023 KDIGO update will likely make cystatin C the preferred method for elderly patients. But right now, most clinics still use creatinine-based calculations.
Medications That Need Special Attention
Not all drugs are created equal. Some are safe even with poor kidney function. Others? They’re ticking time bombs.- Metformin: Used for diabetes. In the U.S., it’s banned if creatinine is above 1.5 mg/dL in men or 1.4 mg/dL in women. But European guidelines allow it with close monitoring. The problem? Metformin itself isn’t cleared by kidneys-but its metabolites can build up and cause lactic acidosis, a life-threatening condition.
- Gabapentin: Used for nerve pain and seizures. Over 80% of it is excreted unchanged by the kidneys. If you’re on 300 mg three times a day and your CrCl is below 30 mL/min, you’re at high risk for dizziness, falls, and confusion. The fix? Drop to 300 mg once daily.
- Allopurinol: For gout. The standard dose is 100 mg daily. But if CrCl is below 10 mL/min, start with 100 mg every other day. Too much can cause severe skin reactions.
- Cefepime: An antibiotic. Standard dose: 1 gram every 6 hours. But if CrCl is 10-29 mL/min, stretch that to every 12 hours. Below 10 mL/min? Once daily. Miss this, and you risk seizures.
- Rivaroxaban: A blood thinner. The dose must drop from 20 mg daily to 15 mg daily if CrCl is 15-49 mL/min. Too high? Risk of major bleeding. Too low? Risk of stroke.
- Lithium: For bipolar disorder. Therapeutic range is 0.6-0.8 mmol/L. Kidneys clear 80% of it. A small drop in kidney function can push levels into toxic territory. Monthly blood tests are non-negotiable.
Some drugs don’t need adjustment at all. Glipizide, for example, is metabolized by the liver. Even with poor kidney function, it’s generally safe. But many prescribers don’t know this-and they avoid it unnecessarily.
Common Dosing Strategies
There are three main ways to adjust for kidney function:- Dose reduction: Lower the amount per dose. Example: Gabapentin drops from 300-1200 mg daily to 100-300 mg daily.
- Interval extension: Keep the same dose but give it less often. Example: Vancomycin goes from every 12 hours to every 48 hours.
- Combination approach: Reduce dose AND extend interval. Example: Piperacillin/tazobactam drops from 3.375g every 6 hours to 2.25g every 8 hours.
The "50% rule"-cut the dose in half if kidney function is below 50 mL/min-is tempting. But it’s dangerous. It doesn’t work for drugs with nonlinear metabolism, like vancomycin. One wrong adjustment can mean the difference between healing and hospitalization.
What Goes Wrong in Real Clinics
Here’s the hard truth: most doctors don’t adjust doses correctly. A 2015 study of 1,200 prescriptions found only 43.7% of elderly patients got the right dose. The worst offenders? Gabapentin (68% wrong), rivaroxaban (52% wrong), and allopurinol (47% wrong). Why? Time pressure. Lack of training. Outdated guidelines. And too many pills to manage. Even worse, many clinics still use serum creatinine alone. They don’t calculate CrCl at all. Or they use MDRD when they should use Cockcroft-Gault. One study showed 30% of dosing errors came from using the wrong equation. And it’s not just doctors. Pharmacists, nurses, and even patients miss these changes. A 78-year-old might take their usual gabapentin dose because "it’s always worked before." They don’t know their kidneys changed.What Works: Real Solutions
The good news? We know how to fix this.- Pharmacist-led reviews: At Mayo Clinic, having clinical pharmacists manage dosing for patients over 65 cut adverse drug events by 58%. They check every med, calculate CrCl, and flag risks.
- Electronic alerts: At the University of Nebraska Medical Center, adding automated alerts in the EHR system reduced dosing errors by 37% in just one year.
- Mobile apps: Tools like Epocrates Renal Dosing are used over a million times a year. They pull in lab values and instantly suggest adjustments.
- AI-powered tools: The FDA-approved DoseOptima platform, launched in 2023, uses real-time lab data to recommend doses with 92.4% accuracy across 15,000 patients.
But access isn’t equal. Academic hospitals use these tools in 87% of cases. Community hospitals? Only 53%. Long-term care facilities? Just 28% have formal protocols.
Regulations and Financial Incentives
The government is starting to pay attention. The FDA now requires all new drugs targeting people over 65 to include specific renal dosing info on their labels. The European Medicines Agency has been stricter since 2017. And CMS penalizes hospitals with high rates of drug-related harm-up to 1% of Medicare payments per bed. The Beers Criteria, updated yearly by the American Geriatrics Society, now lists 32 medications with specific renal dosing rules for seniors. If you’re on one of these and your dose isn’t adjusted, you’re at risk.What You Can Do
If you or a loved one is over 65 and taking any regular meds:- Ask your doctor: "What’s my CrCl?" Not just creatinine.
- Ask: "Are any of my meds cleared by my kidneys? Do they need adjusting?"
- Ask for a medication review with a pharmacist.
- Keep a list of all meds-including supplements-and bring it to every appointment.
- Watch for signs of toxicity: confusion, dizziness, nausea, muscle weakness, or unusual fatigue.
Don’t assume your dose is right because it’s "always been this way." Your body changes. So should your meds.
What’s Next
The future of renal dosing is personal. The NIH is studying how genetics affect how elderly patients clear drugs. A $12.7 million trial is looking at gene variants that change kidney clearance. Soon, we may be able to tailor doses based on your DNA-not just your age or creatinine. The American Society of Health-System Pharmacists is finalizing a national standard for renal dosing across 150 high-risk drugs. That’s huge. Right now, every hospital does it differently. The goal? Prevent 115,000 adverse drug events a year in the U.S. That’s 115,000 falls, hospital stays, and deaths that could be avoided. It’s not about being perfect. It’s about being careful. One small change in a dose can save a life.How do I know if my kidney function is low?
Your doctor should calculate your creatinine clearance (CrCl) using the Cockcroft-Gault equation, which uses your age, weight, sex, and blood creatinine level. A CrCl below 60 mL/min suggests kidney impairment. Many people assume their creatinine is normal, but in older adults, low muscle mass can hide poor kidney function. Ask for the actual CrCl number-not just the creatinine result.
Which medications are most dangerous if not adjusted for kidney function?
Gabapentin, rivaroxaban, allopurinol, digoxin, lithium, and certain antibiotics like cefepime are high-risk. These drugs are cleared mostly by the kidneys. If your kidneys slow down, they build up to toxic levels. Gabapentin can cause confusion and falls. Lithium can cause seizures. Cefepime can trigger seizures at high levels. Never assume a dose is safe just because it’s "standard."
Should I stop taking metformin if I have kidney issues?
In the U.S., metformin is typically stopped if creatinine exceeds 1.5 mg/dL in men or 1.4 mg/dL in women. But newer guidelines allow it with close monitoring if kidney function is only mildly reduced. The risk isn’t metformin itself-it’s lactic acidosis from buildup of its metabolites. If you’re on metformin and have kidney impairment, talk to your doctor about monitoring your blood pH and lactate levels instead of stopping it outright.
Can I use a mobile app to check my medication doses?
Yes. Apps like Epocrates Renal Dosing and DoseOptima are widely used by clinicians and are accurate for most common medications. They link to your lab values and suggest adjustments based on current guidelines. These tools are especially helpful if you’re taking multiple drugs. But always double-check with your pharmacist or doctor before making any changes.
Why do some doctors still give the same dose to elderly patients?
Many don’t know how to calculate kidney function properly. Others rely on serum creatinine alone, which is misleading in older adults. Time pressure, lack of training, and outdated habits also play a role. In long-term care, staff often don’t have access to dosing tools. It’s not negligence-it’s a system problem. But awareness is growing, and tools are improving.
What should I do if I think my dose is too high?
Don’t stop taking the medication on your own. Call your doctor or pharmacist immediately. Write down your symptoms: dizziness, confusion, nausea, weakness, or irregular heartbeat. Ask: "Could this be from my meds? Is my kidney function checked? Should my dose be lowered?" Bring a full list of your medications to your next appointment. You’re your own best advocate.

Andrew McAfee
November 20, 2025My dad was on gabapentin for years and never had his CrCl checked. One day he fell and broke his hip. Turned out his dose was triple what it should’ve been. No one ever told us kidneys change with age. This post saved my ass.
Andrew Camacho
November 20, 2025Let me tell you something real. The system is rigged. Pharma companies don’t want you adjusting doses because they make more money off people getting sick. They push the same pills for everyone. And doctors? They’re too busy scrolling through TikTok between visits to even look at a creatinine number. This isn’t medical negligence-it’s corporate murder with a white coat.
And don’t even get me started on MDRD. That equation was designed for young, muscular men. It’s like using a ruler made for NBA players to measure a toddler. They’re literally killing people with bad math. I’ve seen it. I’ve buried friends because of this. And now you want me to believe AI tools are gonna fix it? Nah. Fix the greed first.
Arup Kuri
November 22, 2025India has this problem too but worse. My uncle took lithium for bipolar and his doctor never checked his kidneys. He ended up in coma for 3 weeks. Doctors here don’t even know what CrCl means. They just write the same script they give to 30 year olds. And no one questions it because elders are silent. They think dying is normal at 70. It’s not normal. It’s criminal.
Also why is everyone using apps like Epocrates? Are we outsourcing our brains now? My cousin uses an app to tell him if his blood pressure is high. What’s next? A robot telling you to breathe?
Elise Lakey
November 23, 2025This is so important. I’ve been quietly asking my mom’s doctor for her CrCl for months. He finally did it last week-turns out it’s 34. I had no idea gabapentin was her biggest risk. I’m going to schedule a pharmacist consult next week. Thank you for giving me the language to ask the right questions.
Erika Hunt
November 24, 2025I just want to say how deeply moved I am by the clarity and compassion in this post. It’s not just clinical information-it’s a lifeline for families who are terrified of watching their parents slip away because of something that could’ve been prevented with a simple calculation. I’ve spent the last three years helping my grandmother navigate her meds, and I can’t tell you how many times we were told, ‘Oh, she’s fine, her creatinine is normal.’ I now know that phrase is a lie wrapped in a lab report. I’ve printed out the Cockcroft-Gault formula and taped it to the fridge. I’ve started keeping a color-coded spreadsheet of her meds, doses, and labs. I’m not a nurse or a doctor, but I’m her advocate. And if this post helps even one person avoid a hospital stay, it’s worth every word.
Also, I love that you mentioned cystatin C. I’ve been reading up on it and I think it’s going to be the future. My sister’s rheumatologist just started using it for her, and the difference in interpretation was night and day. We need this everywhere. Not just in fancy hospitals. In nursing homes. In rural clinics. In every single pharmacy.
And the part about metformin? That changed everything for me. I thought we had to stop it. Now I know we just need to monitor. Thank you for not just listing risks but giving us hope and tools.
prasad gaude
November 25, 2025Back in my village in Kerala, the local doctor gives the same pills to everyone. Old man with no teeth, young boy with a fever, grandmother with three heart meds-all get the same dose. I told my aunt to ask for CrCl. She said, ‘What is this? Some English word?’ I showed her the formula on my phone. She laughed. Said, ‘You think I’m a doctor?’ I cried that night. This isn’t just medicine. It’s dignity. And we’re taking it away slowly, one wrong pill at a time.
Timothy Sadleir
November 26, 2025While I appreciate the intent of this article, I must emphasize that the reliance on computational formulas such as Cockcroft-Gault and MDRD is fundamentally flawed in the absence of standardized, population-specific calibration curves. Furthermore, the uncritical adoption of mobile applications such as Epocrates and DoseOptima represents a dangerous delegation of clinical judgment to algorithmic black boxes that are neither validated nor auditable under the HIPAA framework. The FDA’s endorsement of DoseOptima, while ostensibly progressive, does not mitigate the inherent epistemological risks of automated decision-making in geriatric pharmacotherapy. We must return to first principles: clinical observation, longitudinal monitoring, and physician discretion-not software recommendations.
Srikanth BH
November 28, 2025You’re not alone. I’ve been helping my neighbor, Mrs. Rivera, for a year now. She’s 82, on five meds, and no one ever adjusted her gabapentin. She was falling every week. I found this post, printed it out, and took it to her pharmacist. They changed her dose in 10 minutes. Now she walks without her cane. One small change. One saved life. Keep sharing this stuff. We need more people like you.