18 Nov 2025
- 8 Comments
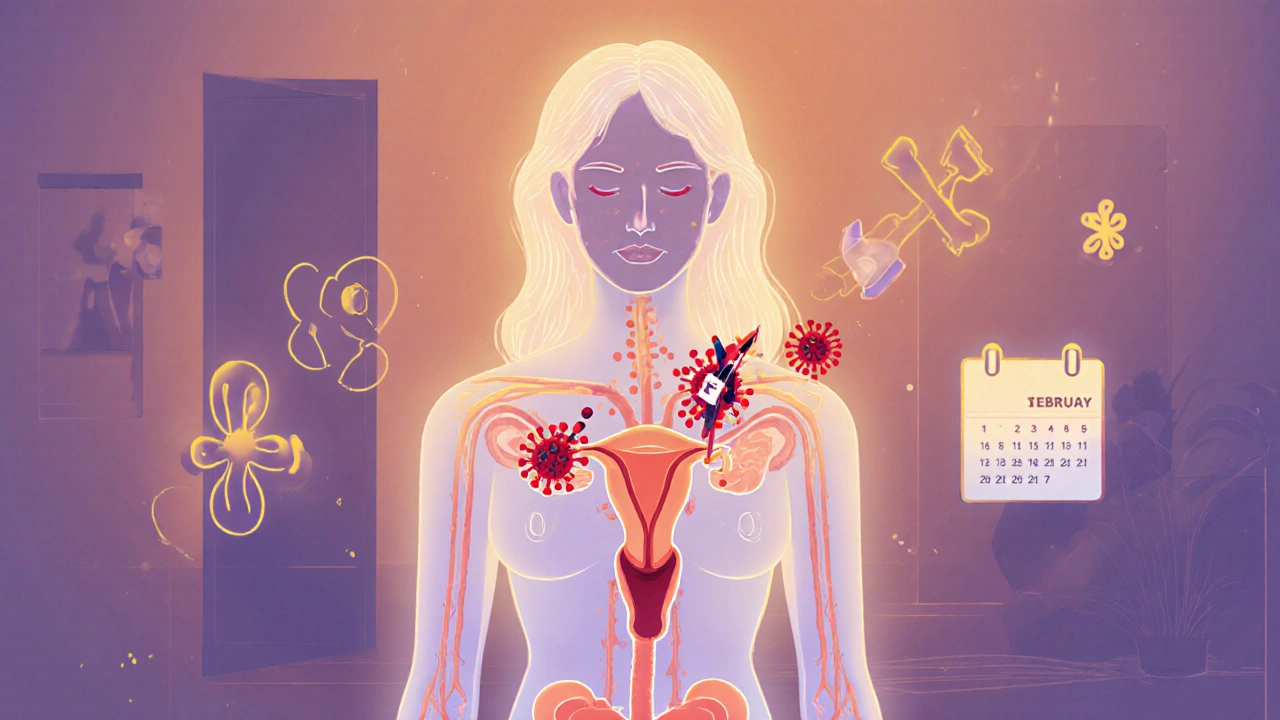
When your period stops for three months or more without pregnancy, menopause, or a clear reason like extreme weight loss, it’s called amenorrhea. For many women, this isn’t just inconvenient-it’s a red flag. And in a growing number of cases, the root cause isn’t stress or diet. It’s an autoimmune disorder quietly attacking the body’s hormonal balance.
What Amenorrhea Really Means
Amenorrhea isn’t a disease. It’s a symptom. Your body isn’t producing the right signals to trigger ovulation and menstruation. That usually means your hypothalamus, pituitary gland, or ovaries aren’t talking to each other properly. Estrogen drops. Progesterone stalls. The uterine lining doesn’t build up. And your period doesn’t come.Primary amenorrhea means you never started your period by age 15. Secondary amenorrhea means you had regular cycles and then they stopped. Most women seeking answers are dealing with secondary amenorrhea. And in up to 15% of these cases, an autoimmune condition is the hidden trigger.
Autoimmune Disorders That Disrupt Your Cycle
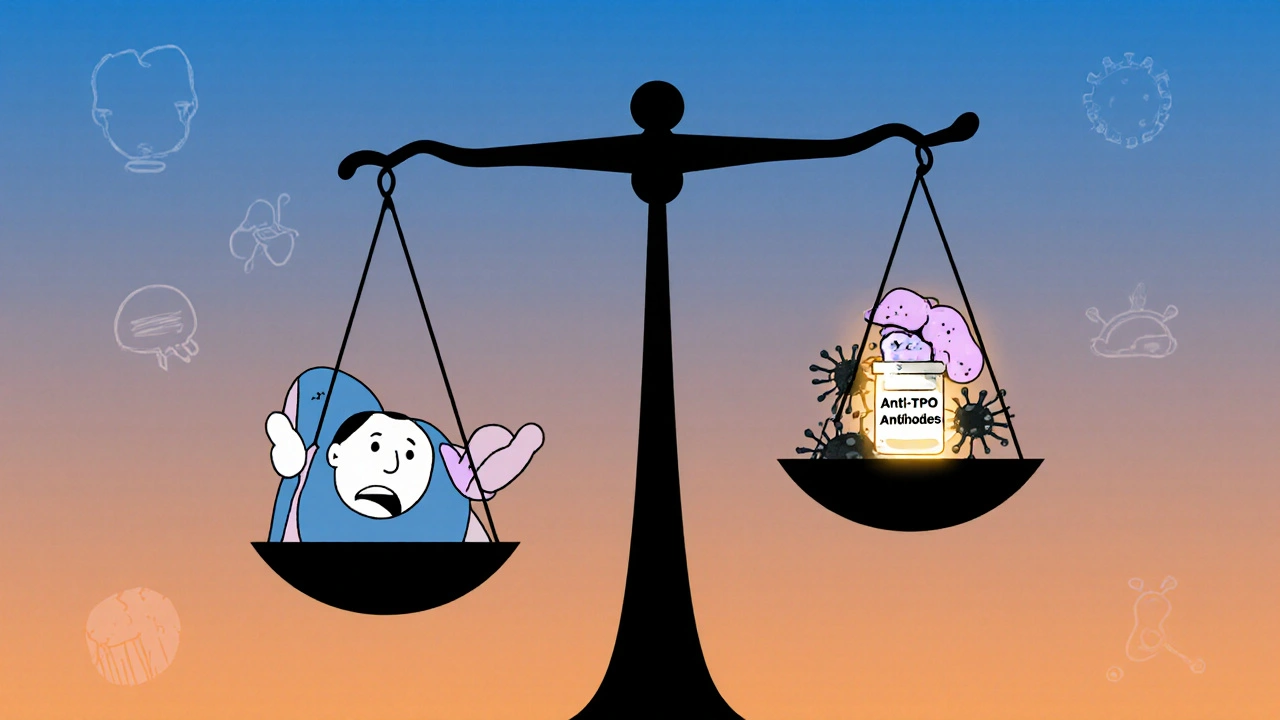
Your immune system is designed to fight viruses and bacteria. But in autoimmune disorders, it turns against your own tissues. When it targets the thyroid, adrenal glands, or ovaries, your menstrual cycle pays the price.Hashimoto’s thyroiditis is the most common link. About 20% of women with unexplained amenorrhea test positive for thyroid antibodies. Even when thyroid hormone levels look normal on a standard TSH test, low-grade inflammation from Hashimoto’s can suppress the hypothalamic-pituitary-ovarian axis. That means your brain stops telling your ovaries to release eggs.
Systemic lupus erythematosus (SLE) doesn’t just cause joint pain and rashes. It can trigger premature ovarian insufficiency. Studies from the American College of Rheumatology show that women with lupus are three times more likely to experience early menopause or amenorrhea than those without it. The immune system attacks ovarian follicles, reducing egg supply and hormone output.
Autoimmune oophoritis is rare but direct. In this condition, the immune system specifically targets the ovaries. Antibodies bind to ovarian tissue, causing inflammation and scarring. Many women don’t know they have it until they’re tested for infertility or amenorrhea. A 2023 study in Human Reproduction found that 12% of women under 35 with unexplained amenorrhea had ovarian antibodies.
Addison’s disease, or primary adrenal insufficiency, also plays a role. When your adrenal glands don’t make enough cortisol and aldosterone, your body shifts into survival mode. Reproduction becomes a low priority. Estrogen production drops. Periods vanish. This isn’t just about stress-it’s about hormone starvation.
Why the Connection Exists
The immune system and the endocrine system are deeply linked. They share signaling molecules. Inflammation from autoimmune activity raises cytokines like IL-6 and TNF-alpha. These molecules interfere with GnRH-the hormone your hypothalamus releases to start the menstrual cycle. Less GnRH means less FSH and LH. Less FSH and LH means no ovulation. No ovulation means no period.Genetics also matter. Women with one autoimmune condition are far more likely to develop another. If you have type 1 diabetes or celiac disease, your risk of developing autoimmune thyroid disease or ovarian failure increases significantly. The same faulty immune regulation that destroys insulin-producing cells can also target ovarian tissue.
What Your Doctor Might Miss
Too often, doctors treat amenorrhea like a lifestyle issue. They ask about weight, exercise, stress, or birth control. They might check for polycystic ovary syndrome (PCOS). But if you’re lean, active, and not on the pill-and your period still disappeared-you need deeper testing.Standard hormone panels often miss autoimmune causes. A normal TSH doesn’t rule out Hashimoto’s. You need anti-TPO and anti-thyroglobulin antibodies. A normal FSH and LH doesn’t rule out ovarian damage-you need anti-ovarian antibody tests. Estradiol might be low, but without checking for antibodies, you won’t know why.
Many women go years without answers. One patient I spoke with in Melbourne had her period stop at 28. She was told she was "too stressed". She changed jobs, started yoga, ate better. Nothing worked. Two years later, after a miscarriage and a thyroid antibody test, she was diagnosed with Hashimoto’s. Her period returned within six months of starting thyroid medication.
How to Get Tested
If you’ve had amenorrhea for more than three months and other causes are ruled out, ask for these tests:- Thyroid peroxidase antibodies (anti-TPO)
- Thyroglobulin antibodies (anti-Tg)
- Follicle-stimulating hormone (FSH) and luteinizing hormone (LH) levels
- Estradiol (E2)
- Anti-ovarian antibodies (if available through a specialist)
- Adrenal antibodies (17-alpha-hydroxylase, 21-hydroxylase) if you have fatigue, low blood pressure, or salt cravings
- ANA (antinuclear antibody) screen for lupus or other systemic conditions
Don’t stop at TSH. Many clinics still treat thyroid disease based on TSH alone. But in autoimmune-related amenorrhea, even slightly elevated antibodies-without full hypothyroidism-can be enough to disrupt your cycle.
What Treatment Looks Like
There’s no magic pill to stop autoimmunity. But you can manage it. And when you do, your period often comes back.For Hashimoto’s: Thyroid hormone replacement (levothyroxine) usually restores cycles within 3-6 months. Some women need higher doses than standard guidelines suggest because their bodies are more sensitive to low estrogen.
For lupus or ovarian inflammation: Immunosuppressants like low-dose prednisone or hydroxychloroquine may be used. These don’t cure the disease, but they reduce inflammation enough to let the ovaries recover. In some cases, hormone therapy (estrogen and progesterone) is added to rebuild the uterine lining while the immune system calms down.
For adrenal insufficiency: Cortisol replacement (hydrocortisone) is essential. Without it, your body stays in survival mode. Periods won’t return until cortisol levels are stable.
Diet and lifestyle help, but they’re not enough on their own. Cutting gluten can improve symptoms in women with both celiac disease and amenorrhea. Reducing processed sugar and inflammation triggers supports immune balance. But if the autoimmune fire is burning, you need medical treatment to put it out.

When to See a Specialist
If you’ve had amenorrhea for more than six months and standard tests came back normal, it’s time to see a reproductive endocrinologist or a rheumatologist with experience in women’s health. General gynecologists aren’t trained to connect autoimmune markers with menstrual loss.Look for clinics that offer combined endocrine-immunology care. In Melbourne, several private practices now have multidisciplinary teams that test for antibodies alongside hormone panels. Don’t settle for a one-off blood test. Ask for a full autoimmune workup.
What This Means for Fertility
Amenorrhea from autoimmune causes can affect fertility-but not always permanently. If ovarian damage is early, restoring hormone balance can bring back ovulation. If the ovaries are already scarred, IVF with donor eggs may be needed.But here’s the good news: treating the autoimmune condition first often improves outcomes. Women with Hashimoto’s who get their thyroid levels optimized before trying to conceive have higher pregnancy rates and lower miscarriage risk. The same goes for lupus-stable disease before pregnancy leads to healthier outcomes.
Don’t assume infertility is inevitable. Test. Treat. Try again.
What You Can Do Today
If your period has disappeared and you suspect an autoimmune link:- Write down your symptoms: fatigue, dry skin, hair loss, joint pain, rashes, or digestive issues.
- Track your cycle history: When did it stop? Was there a trigger like infection, stress, or surgery?
- Ask for antibody tests-not just hormone levels.
- Don’t ignore subtle signs. A single missed period isn’t an emergency. Three or more is a warning.
- Find a doctor who listens. If they say it’s "just stress," ask for a second opinion.
Your body isn’t broken. It’s signaling something deeper. Autoimmune disorders don’t just affect your joints or skin. They can silence your cycle. But when you uncover the real cause, recovery is possible.
Can stress cause amenorrhea the same way autoimmune disorders do?
Yes, stress can cause functional hypothalamic amenorrhea by suppressing GnRH. But the key difference is reversibility. Stress-related amenorrhea often returns with reduced exercise, better nutrition, and lower cortisol. Autoimmune amenorrhea doesn’t improve with lifestyle alone-it needs medical treatment to calm the immune system. If your period doesn’t come back after addressing stress, autoimmunity should be ruled out.
Can you have autoimmune amenorrhea without other symptoms?
Absolutely. Many women with Hashimoto’s or early autoimmune oophoritis have no classic symptoms like fatigue or joint pain. The only sign is missed periods. That’s why testing for antibodies is critical-even if you feel fine. Silent autoimmunity is common, especially in young women.
Does birth control mask autoimmune amenorrhea?
Yes. Birth control pills force a withdrawal bleed, which looks like a period but isn’t natural ovulation. This can hide the fact that your body isn’t producing estrogen or ovulating on its own. If you’re on the pill and your period stops during the placebo week, it doesn’t mean your cycle is healthy. Stopping the pill is often the first step in diagnosing underlying autoimmune causes.
Is amenorrhea from autoimmunity permanent?
Not always. If caught early and treated, many women regain regular cycles. But if ovarian tissue is destroyed or the adrenal glands are severely damaged, recovery may not happen without hormone replacement. The earlier you test and treat, the better your chances of restoring natural function.
Can diet cure autoimmune amenorrhea?
No. While anti-inflammatory diets can reduce overall immune activation, they don’t stop antibody production or reverse tissue damage. You still need medical treatment. Diet supports recovery but doesn’t replace it. Think of it like taking insulin for type 1 diabetes-it doesn’t cure the disease, but it keeps you alive and functioning.

Jenny Lee
November 18, 2025This changed everything for me. My period vanished for 8 months and everyone said it was stress. Turns out I had Hashimoto’s. Started levothyroxine and boom-cycle returned in 4 months. No yoga, no kale smoothies, just meds.
Stop blaming yourself.
Jeff Hakojarvi
November 20, 2025Hey i just wanna say thank you for this post. i had no idea autoimmune stuff could do this. my sister went years without a period and they kept telling her to lose weight or chill out. she finally got tested after a miscarriage and turned out she had anti-ovarian antibodies. she’s on hydroxychloroquine now and her cycle’s back. i wish more docs knew this. also typo: ‘luteinizing’ was spelled ‘lutenizing’ once but you get the point lol.
please keep sharing stuff like this.
Timothy Uchechukwu
November 20, 2025So now we’re blaming women’s bodies for not working because of some invisible immune system drama? In my country we don’t have time for this overmedicalization. Women used to just deal with irregular cycles. Back in Nigeria we had 7 kids and still farmed. No blood tests no hormones just grit. This is what happens when you let science become a religion.
Stop making women feel broken for being women.
Ancel Fortuin
November 22, 2025Of course it’s autoimmunity. Did you know the CDC is hiding the truth? Big Pharma doesn’t want you to know that glyphosate in your Cheerios is triggering ovarian antibodies. They’d rather sell you levothyroxine than admit Roundup is turning women into walking hormone corpses. And don’t get me started on how birth control is a government mind-control tool to mask the real problem.
They’re silencing your cycle so they can silence your voice.
Hannah Blower
November 23, 2025How quaint. You’ve reduced the profound neuroendocrine-immune axis to a checklist of lab values and pharmaceutical band-aids. The real issue isn’t antibodies-it’s the ontological collapse of feminine embodiment in a capitalist medical-industrial complex that commodifies fertility and pathologizes natural variation.
You treat the symptom because you refuse to confront the systemic violence of patriarchal medicine. Your ‘treatment’ is just another form of epistemic erasure wrapped in a white coat.
And yes, I’ve read the 2023 Human Reproduction paper. You haven’t.
Try reading Irigaray before you prescribe hydrocortisone.
Gregory Gonzalez
November 24, 2025Wow. Someone actually wrote a post that doesn’t start with ‘as a woman who’s been there’ and ends with ‘just take supplements’. Impressive. Most of these articles are just glorified Instagram captions with medical jargon slapped on.
But let’s be real-how many of these antibody tests are even covered by insurance? Or available outside of fancy coastal clinics? You’re preaching to the converted, the ones who can afford to see a reproductive endo who speaks fluent Latin.
For the rest of us? We’re still waiting for our TSH results from the county clinic.
Ronald Stenger
November 24, 2025Let’s not pretend this is just about hormones. The decline in female fertility across the West isn’t random. It’s a biological response to cultural decay. Women are overworked, overstimulated, over-medicated, and underfed real food. The immune system isn’t attacking the ovaries-it’s rejecting the entire modern lifestyle.
And now we’ve got people running to labs for antibody tests instead of asking why their daughter’s eating processed junk and sleeping 4 hours a night.
Stop looking for a pill. Look in the mirror.
Samkelo Bodwana
November 25, 2025I come from a small town in South Africa where most women don’t have access to labs or specialists. But I’ve seen this firsthand-women with no periods, no diagnosis, just silence. I once met a nurse who told a 24-year-old she was ‘too thin to bleed’ and sent her home. Two years later she was diagnosed with lupus and had lost nearly all ovarian reserve.
This post is vital. Not because it’s perfect, but because it gives language to something that’s been buried. I don’t care if it’s Hashimoto’s or glyphosate or patriarchy-what matters is that someone finally said: ‘This isn’t normal, and you deserve to know why.’
Let’s not fight over the cause. Let’s fight for the access. Every woman, everywhere, deserves a chance to get tested. Even if it’s just one antibody panel. Even if it’s in a clinic with no air conditioning. Even if it costs $10.
Let’s not let privilege be the gatekeeper of health.