7 Feb 2026
- 13 Comments
Side Effect Prioritization Tool
Understand Your Priorities
When choosing medication, it's not about side effects alone, but which side effects matter most to YOU. This tool helps you identify your personal priorities so you can have more meaningful conversations with your doctor.
Side Effects to Consider
Check the side effects that matter to you, then drag and drop to prioritize them.
Your Priorities
Drag side effects to rank them from most to least important. Your priority order will help guide your decision.
Start by dragging side effects here to rank them.
How Your Priorities Impact Your Treatment
Understanding your priorities helps you and your doctor choose the best treatment option. Here's what your ranking means:
Select side effects and prioritize them to see how they affect treatment choices.
When you’re prescribed a new medication, you’re not just getting a pill. You’re getting a trade-off. A chance to feel better - but also a chance to deal with nausea, fatigue, dizziness, or worse. And too often, patients are left to guess what those trade-offs really mean. That’s where shared decision-making scripts come in. They’re not just fancy doctor talk. They’re real tools that help you and your clinician talk through what matters most: your life, your comfort, and what side effects you’re willing to live with.
Why Side Effects Aren’t Just Numbers
You’ve probably heard phrases like "this side effect is rare" or "most people tolerate it fine." But those words don’t tell you what it actually feels like. One out of ten people get nausea? That sounds harmless - until you’re the one vomiting every morning and can’t hold down breakfast, let alone go to work. That’s why shared decision-making shifts the focus from statistics to your experience. A 2021 study in the Journal of General Internal Medicine found that when patients used structured conversations about side effects, their decisional conflict dropped by 23%. That means less anxiety, fewer second-guesses, and more confidence in sticking with a treatment. The key? Talking about side effects as real, personal risks - not abstract percentages.The SHARE Approach: A Step-by-Step Framework
The Agency for Healthcare Research and Quality (AHRQ) created the SHARE Approach to give clinicians a clear, repeatable way to have these conversations. It’s not a script you memorize - it’s a rhythm you learn.- Seek opportunities: Start by asking, "Do you have any concerns about how this medication might affect your daily life?" Not "Do you have any questions?" - that’s too vague.
- Help explore options: Lay out the alternatives. Maybe there are two pills that treat the same condition, but one causes drowsiness and the other causes dry mouth. Which matters more to you?
- Assess values: This is the heart of it. Ask: "Some people are more worried about weight gain, while others can’t handle constant fatigue - what’s most important to you?"
- Reach a decision: Don’t just pick the option. Say: "So if we go with this, you’re okay with mild dizziness but want to avoid any sleepiness?" Confirm it out loud.
- Evaluate: Follow up: "How’s the medication treating you? Any surprises?" This isn’t a one-time talk.
This isn’t theory. At Scripps Health, doctors using this method saw a 22% drop in follow-up visits because patients weren’t calling in confused or upset about side effects they weren’t prepared for.
The Three-Talk Model: Clear Language, Clearer Risks
Another powerful tool is the three-talk model used by the American Academy of Family Physicians. It breaks down the conversation into three clear parts:- Option talk: "Here are the two choices we have. One reduces your risk of stroke by 30%, but 1 in 10 people get serious bleeding. The other doesn’t affect bleeding risk, but only cuts stroke risk by 15%."
- Decision talk: "Which outcome matters more to you - avoiding stroke or avoiding bleeding?"
- Preference talk: "What would make you say ‘no’ to this treatment?" This is where you find out if insomnia, weight gain, or memory fog is a deal-breaker.
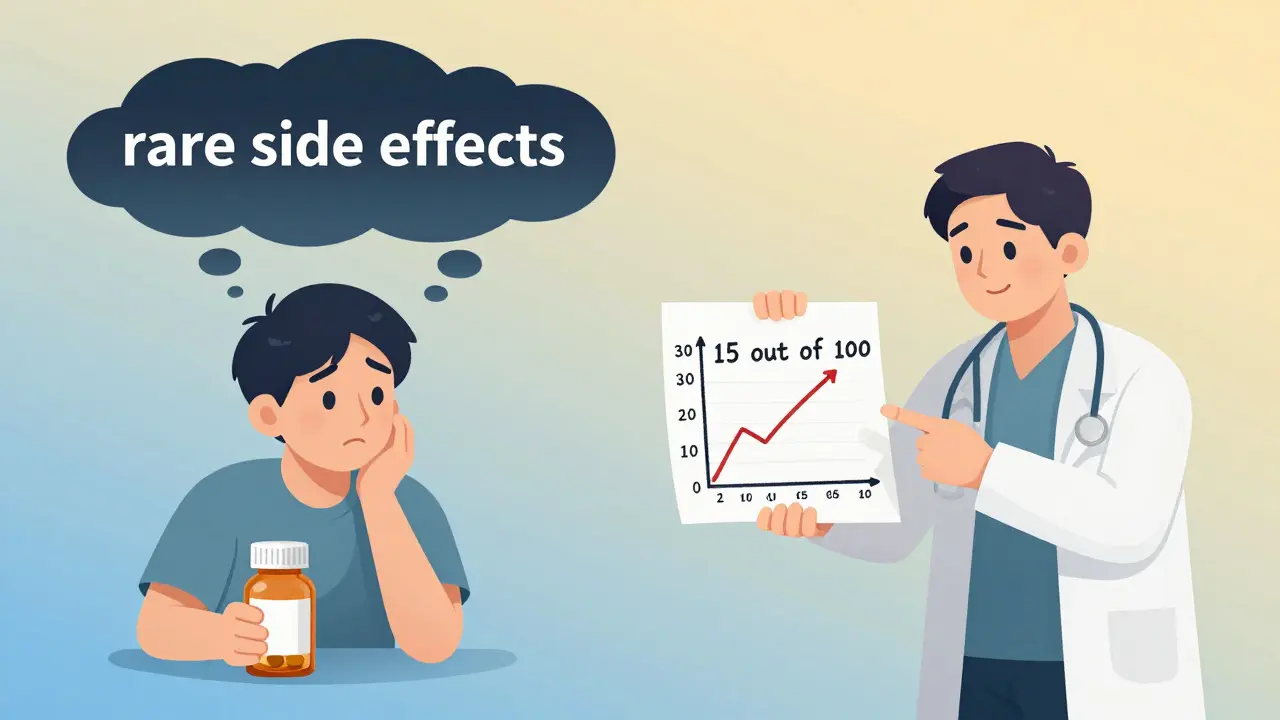
Research in the Annals of Internal Medicine shows patients understand risks 37% better when you use absolute numbers - like "15 out of 100 people" - instead of vague terms like "rare" or "common."
Real-Life Trade-Offs: Statins, Blood Thinners, and More
Some medications force tough choices. For example:- Statins: 86% of people who stop taking them do so because of muscle pain or fatigue. But for someone with a history of heart attack, the benefit can be life-saving. The question isn’t "Is this side effect bad?" It’s "Is it bad enough to risk another heart attack?"
- Anticoagulants: Warfarin or apixaban? One needs regular blood tests. The other costs more but doesn’t. One has a 3-5% annual risk of major bleeding. The other has 2-4%. Which risk do you accept? And how do you feel about carrying an emergency card?
- Antidepressants: Weight gain? Sexual side effects? Sleepiness? One patient might say, "I’ll take the weight gain if I can finally sleep through the night." Another says, "I can’t live with losing my sex drive."
These aren’t just medical decisions. They’re personal ones. And they’re not one-size-fits-all.
What Doesn’t Work - And Why
Not every doctor uses these scripts well. Some read them like a checklist. That’s worse than not using them at all. A 2022 Medscape survey found that 63% of patients felt frustrated when clinicians "just read from a script" without listening. Patients don’t want robotic questions. They want to feel heard. One Reddit user wrote: "My doctor asked, ‘What side effects worry you?’ and I said, ‘I can’t handle feeling tired all day.’ He just nodded and wrote it down. Then he prescribed the one that causes fatigue. I felt like I wasn’t even there." The problem isn’t the script. It’s the delivery. If the conversation feels like a form to fill out, trust breaks down.How to Get Better at This - As a Patient
You don’t have to wait for your doctor to bring this up. You can start the conversation:- "What side effects do most people have with this?"
- "Which ones are serious enough to make you stop taking it?"
- "What would make you say this isn’t worth it?"
- "Can you show me the numbers? Not just ‘rare’ - how many out of 100?"
- "If you were me, what would you choose?"
Many clinics now offer pre-visit decision aids - short videos or handouts that explain side effects before the appointment. These cut consultation time by over 3 minutes, according to Scripps Health. Ask if your clinic has them.
The Bigger Picture: Why This Matters Now
This isn’t just about better conversations. It’s about better outcomes. A 2021 JAMA Internal Medicine study showed patients who had structured SDM talks were 29% less likely to quit their treatment because of unexpected side effects. And it’s getting official. In 2023, Medicare Advantage plans had to start documenting shared decision-making for high-risk drugs. The American Medical Association now has a billing code (96170-96171) that pays doctors $45-$65 for these conversations. Epic Systems - the most common electronic health record platform - rolled out built-in SDM scripts in 2022. They’re now active in 63% of U.S. hospitals. That means if you’re seeing a doctor in a major hospital system, this isn’t optional anymore.What’s Next?
Artificial intelligence is starting to help. In 2023, the NIH funded research to build tools that listen to doctor-patient conversations and flag when side effect concerns aren’t being addressed. Imagine a system that quietly reminds a clinician: "You haven’t asked about sleep disruption yet." The goal isn’t to replace human talk. It’s to make sure no one walks out of a clinic thinking, "I didn’t know it would be this hard."Final Thought
Your body, your life, your priorities. No one else can decide what side effects you can live with. But you need the right tools - and the right conversation - to make that call. Shared decision-making isn’t about being told what to do. It’s about being helped to choose what’s right for you.What exactly is shared decision-making for side effects?
Shared decision-making is a structured conversation between you and your clinician where you both discuss treatment options, the risks and benefits of each - including side effects - and choose a path based on what matters most to you. It’s not about the doctor deciding for you. It’s about you being an equal partner in choosing what’s best for your life.
Why do doctors sometimes skip discussing side effects?
Time pressure is the biggest reason. Many clinics have 15-minute slots, and doctors feel they need to cover diagnosis, prescriptions, and follow-up. Some also fear scaring patients or causing anxiety. But research shows that when side effects are discussed clearly upfront, patients are more likely to stick with treatment - saving time in the long run.
Can I ask my doctor to use a decision script?
Absolutely. You can say: "I’ve heard about shared decision-making tools that help people understand side effects better. Could we use one of those today?" Many clinics now have them built into their systems. Even if they don’t, most clinicians will adapt to your request - especially if you’re clear about what you want to know.
Are side effect numbers really that important?
Yes. Terms like "rare" or "common" mean different things to different people. Saying "1 in 10 people get nausea" is clearer than "some people experience nausea." Studies show patients understand risks 37% better when they’re given absolute numbers. That helps you weigh whether the side effect is worth the benefit - for you.
What if I’m not sure which side effect matters most?
That’s normal. Ask: "What’s the most common side effect that makes people stop this medication?" Or: "If you were in my situation, which side effect would you find hardest to live with?" Often, hearing someone else’s experience helps you clarify your own priorities. You don’t need to have all the answers - just the willingness to explore them together.


Patrick Jarillon
February 7, 2026Let me guess... this whole 'shared decision-making' thing is just Big Pharma's way of making you feel guilty for not taking your pills. 🤡 They know you're scared of side effects, so they give you a script to make you think you're in control. Meanwhile, your insurance company is still hiking up your copay. This isn't empowerment-it's a distraction tactic. I've seen doctors read these scripts like they're reciting a prayer. No one's actually listening. Wake up, people. This is capitalism in a lab coat.
Eric Knobelspiesse
February 8, 2026idk man i think this is kinda cool but also kinda overengineered? like sure, '1 in 10 get nausea' sounds better than 'some people' but honestly most folks just want the doc to say 'this might make you feel like crap for a week but you'll be better after' and then hand them the script. i mean, do we really need a 5 step framework? we're not launching a rocket. also typo: 'apixaban' is spelled right but i keep thinking it's 'apixabam' lmao
Heather Burrows
February 10, 2026I find it deeply concerning that we’re now turning deeply personal medical decisions into structured checklists. There’s a quiet dignity in suffering in silence, you know? To force patients into naming their fears-'what’s most important to you?'-is to weaponize vulnerability. And don’t get me started on billing codes. Now doctors are incentivized to perform empathy. How profoundly sad. This isn’t patient-centered care. It’s emotional labor commodified.
Ritu Singh
February 10, 2026As someone raised in a culture where elders are never questioned, this concept is revolutionary. In India, we are taught to trust the doctor implicitly. But I have seen too many young people suffer silently because they were too afraid to say, 'I cannot live with this side effect.' This framework, though Western, carries a universal truth: dignity in choice. I have shared this with my niece, who is now asking her psychiatrist about sexual side effects-not because she was told to, but because she felt seen. This is not a script. It is a permission slip to be human.
Mark Harris
February 11, 2026YESSSS this is the stuff! I’ve been on 3 different meds in the last 5 years and NONE of my docs ever asked me what mattered. I just got handed prescriptions like a vending machine. Finally had one who said 'what would make you say no?' and I was like 'if I can’t dance at my sister’s wedding, I’m not taking it.' She got it. We switched meds. I danced. Life changed. You don’t need a 10-page pamphlet. You need one person who asks the right question. 🙌
Savannah Edwards
February 11, 2026I think what’s missing from this whole conversation is the emotional weight of side effects-not just their frequency, but their texture. It’s not just 'fatigue.' It’s the kind of fatigue where you stare at your child’s drawing on the fridge and think, 'I wish I had the energy to hug them.' It’s not just 'dry mouth'-it’s the humiliation of sipping water during a job interview because your tongue feels like sandpaper. These scripts help, yes, but only if the clinician pauses long enough to let the silence breathe. The real magic isn’t in the structure-it’s in the space between the words.
Jesse Lord
February 11, 2026i love that this exists but honestly the biggest problem is time. my doc has 8 minutes per patient. theyre not gonna do a 5 step script. theyre gonna say 'you good?' and you say 'yeah' and then you get the thing that makes you vomit. the system is broken. scripts dont fix that. funding more time does. also i like that they mention epic systems. that means its probably gonna be forced into every chart now. which is both good and terrifying
Lakisha Sarbah
February 12, 2026I’m glad this is being talked about, but I wish we’d talk more about how race and class play into this. My sister, who’s Black, got told 'most people tolerate this' when she asked about dizziness. She ended up in the ER. My white friend, same med, same symptoms, got offered alternatives right away. The script doesn’t fix bias. It just makes it look nicer. We need training on implicit bias too-not just conversation templates.
Ariel Edmisten
February 12, 2026Simple. Ask: 'What’s the one side effect you’d hate the most?' Then listen. No scripts needed. Just care.
Niel Amstrong Stein
February 13, 2026bro this is actually 🔥 i didnt think docs would ever care about this stuff. i had a doc last year who literally asked 'if you could pick one side effect to avoid, what would it be?' i said 'no more crying for no reason' and she switched me. i cried again but this time it was from relief. 🥹 also i love that they said 'if you were me'-that one line changed everything. we need more of this. also emojis are life
Paula Sa
February 14, 2026I think this is beautiful. I’ve been on antidepressants for 12 years, and the moment I finally said, 'I can’t live without my sex drive,' my doctor didn’t flinch. She said, 'Let’s try something else.' That moment-that quiet, patient, non-judgmental space-was more healing than any pill. It’s not about the framework. It’s about the person on the other side of the table choosing to see you.
Mary Carroll Allen
February 14, 2026okay but like... why is it always the patients who have to push for this? why isnt the system just built this way from the start? why do we have to ask 'can we use a decision aid?' like its a favor? also typo: 'apixaban' again lol. also i just wanna say i cried reading the statin part. i lost my dad to a heart attack and i refused his statin because i was scared of muscle pain. i wish someone had said 'what’s the one thing you’d give up to live?' instead of just handing me a paper. this is so important. i’m sharing this everywhere.
Joey Gianvincenzi
February 16, 2026The institutionalization of shared decision-making is a necessary evolution in patient autonomy. However, the reliance on standardized scripts risks reducing complex human experiences to algorithmic templates. Furthermore, the introduction of billing codes-while financially incentivizing clinicians-creates a perverse incentive structure wherein the act of listening becomes transactional. This is not patient empowerment. It is bureaucratic co-optation dressed in compassionate language. We must preserve the sanctity of the therapeutic encounter-not commodify it.