7 Dec 2025
- 12 Comments
Managing bipolar disorder isn’t about finding one magic pill. It’s about balancing two powerful classes of drugs-mood stabilizers and antipsychotics-to keep highs and lows from taking over your life. For many people, this balance is fragile. One wrong dose, one missed blood test, or one ignored side effect can send you back into a depressive spiral or a manic episode. The goal isn’t just to reduce symptoms-it’s to help you live without constant fear of the next mood crash.
What Mood Stabilizers Actually Do
Mood stabilizers are the backbone of long-term bipolar treatment. Lithium, approved by the FDA in 1970, is still the most studied and trusted option. It doesn’t just calm mania-it reduces suicide risk by 80% compared to no treatment. That’s not a small number. It’s life-saving.
But lithium isn’t simple. You need regular blood tests. When you start, you might get tested weekly. Once stable, every two to three months. The target range? Between 0.6 and 1.0 mmol/L. Too low, and it won’t work. Too high-above 1.2 mmol/L-and you risk toxicity. Symptoms? Slurred speech, shaking hands, confusion. Seizures, even.
Side effects are real. Thirty to forty percent of people on lithium drink three liters of water a day just to stay hydrated. Hand tremors? Common. Weight gain? Average 10 to 15 pounds in the first year. Nausea? Happens to one in five. Some people switch because of this. Others stick with it because the alternative-weekly suicidal thoughts-is worse.
Other mood stabilizers include valproate, carbamazepine, and lamotrigine. Valproate works fast for mania but carries a black box warning for birth defects. Lamotrigine is the go-to for depression, with a 47% response rate, but it can cause a rare, dangerous rash in 10% of users. That’s why you start low-25mg a day-and increase slowly over weeks.
Antipsychotics: Fast Relief, Heavy Costs
Antipsychotics like quetiapine (Seroquel), olanzapine, and aripiprazole weren’t designed for bipolar disorder. But they work. Fast. Where lithium takes two weeks to show results, quetiapine can start helping in as little as seven days. That’s why they’re often used in acute episodes-when someone is in crisis, hallucinating, or dangerously impulsive.
But the trade-off is steep. Quetiapine causes drowsiness in 60 to 70% of users. Olanzapine leads to an average weight gain of 4.6kg in just six weeks. That’s more than 10 pounds. And with that weight comes risk: 20 to 30% higher chance of type 2 diabetes. Metabolic syndrome-high blood sugar, bad cholesterol, belly fat-isn’t just a side effect. It’s a long-term health threat.
One Reddit user wrote: “I gained 22 pounds on quetiapine. I stopped working out. I felt like a stranger in my own body.” That’s not uncommon. PatientsLikeMe data shows 68% of users report weight gain, with an average of 22 pounds. Tolerability scores? Just 2.8 out of 5.
Yet for some, it’s worth it. A 2023 study found that 70% of treatment-resistant cases improved when antipsychotics were added to a mood stabilizer. The catch? Side effects jump by 25 to 30%. You’re trading one set of problems for another.
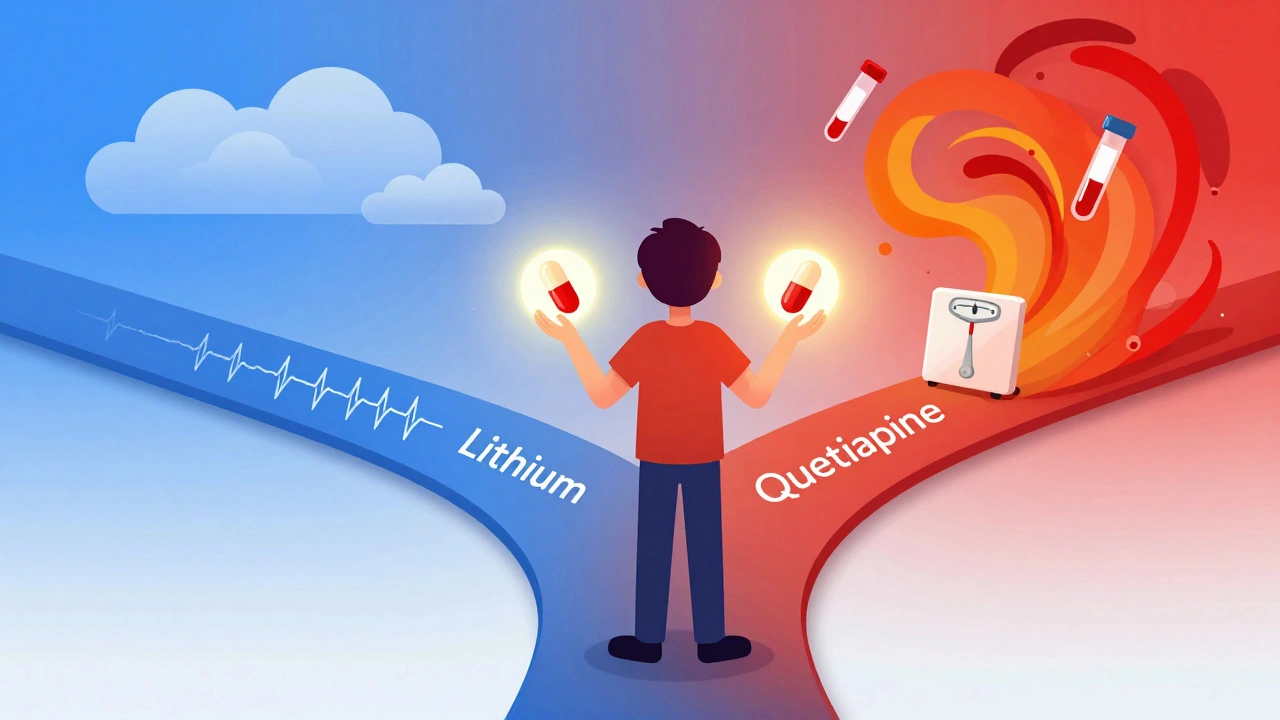
Lithium vs. Quetiapine: The Real Choice
Let’s compare the two most common drugs head-on.
| Factor | Lithium | Quetiapine |
|---|---|---|
| Best for | Long-term prevention, suicide reduction | Acute mania and depression, fast relief |
| Time to work | 10-14 days | 5-7 days |
| Weight gain | 10-15 lbs in first year | 15-25 lbs common |
| Metabolic risk | Low | High (diabetes, cholesterol) |
| Blood monitoring | Weekly → quarterly | Not required |
| Common side effects | Thirst, tremors, nausea | Sedation, dizziness, dry mouth |
| Relapse prevention | 47% over 12 months | 35% over 12 months |
Some people choose lithium because they want to live longer. Others pick quetiapine because they can’t wait two weeks to feel better. Neither is wrong. But you need to know what you’re signing up for.

The Antidepressant Trap
Many people with bipolar disorder are prescribed antidepressants like fluoxetine or sertraline. It makes sense-depression is crushing. But here’s the catch: antidepressants can trigger mania in 10 to 15% of cases. In some, the risk is as high as 25%.
That’s why experts insist: if you take an antidepressant, you must be on a mood stabilizer too. Never alone. A 2006 study found fluoxetine had a 50.7% response rate in bipolar depression-but only when paired with lithium or valproate. Without it, you’re playing Russian roulette with your mood.
Some doctors still prescribe them. Others, like Dr. Gary Sachs from Harvard, say avoid them entirely unless the depression is life-threatening. Dr. David Miklowitz at UCLA disagrees-he says cautious use, with close monitoring, can help. There’s no universal rule. It depends on your history, your symptoms, your tolerance.
What No One Tells You About Taking These Drugs
Medication management isn’t just about pills. It’s about daily habits.
- Take lithium with food. It cuts nausea by half.
- Split your dose. Two smaller doses a day (morning and night) often feel better than one big one.
- Use metformin if you’re gaining weight on antipsychotics. It’s not approved for this, but 60% of clinicians use it off-label-and patients report losing 5 to 10 pounds over six months.
- Drink water, but don’t overdo it. Too much fluid can dilute lithium and make it less effective. Too little, and you risk toxicity.
- Avoid NSAIDs like ibuprofen or naproxen. They can spike lithium levels by 25 to 60%. Use acetaminophen instead for pain.
And don’t ignore the mental side effects. Cognitive fog? Common. Memory lapses? Frequent. One user said: “I forgot my daughter’s birthday. I wasn’t depressed. I wasn’t manic. I was just… gone.” That’s not weakness. That’s the drug.
What’s New in 2025
The field is changing. In 2023, the FDA approved lumateperone (Caplyta) for bipolar depression. It works as well as quetiapine-but with almost no weight gain. Just 0.8kg in six weeks, compared to 3.5kg for quetiapine.
Long-acting injectables are growing too. Abilify Maintena is a monthly shot of aripiprazole. No daily pills. No forgetting doses. For people who struggle with adherence, it’s a game-changer.
And now, genetic testing is starting to help. Companies like Genomind test for CYP2D6 and CYP2C19 enzyme variants-genes that affect how your body processes 40% of bipolar meds. In trials, this testing improved medication selection accuracy by 30%. By 2027, experts say it’ll be standard.
But here’s the hard truth: even with all this, only 35% of people with bipolar disorder reach full remission. Six in ten still suffer from side effects that make them want to quit.
When to Call Your Doctor
You don’t need to wait for a crisis. Call if:
- Your hands shake more than usual (tremors over 2mm amplitude)
- You’re drinking more than 4 liters of water a day and still thirsty
- Your waistline has grown more than 2 inches in 3 months
- You feel unusually tired, confused, or foggy for more than a week
- You’re having thoughts of self-harm again
These aren’t minor complaints. They’re signals. Your doctor needs to adjust your dose, switch your drug, or add something to protect you.
Final Reality Check
There’s no perfect drug. No easy fix. Lithium saves lives but drains your energy. Quetiapine brings quick relief but steals your body. Lamotrigine helps depression but can give you a rash that lands you in the ER.
But here’s what works: knowing your numbers. Tracking your weight. Writing down your moods. Talking to your doctor every time something changes. And most of all-sticking with it, even when it’s hard.
One Reddit user, after three failed meds, wrote: “Lithium gave me 15 extra pounds. But I haven’t had a suicidal week in 18 months. That’s worth it.”
That’s the real goal. Not to be perfect. Not to feel nothing. Just to feel like yourself-for long stretches, without fear.
Can I stop my bipolar medication if I feel fine?
No. Stopping suddenly can trigger a severe relapse, sometimes worse than before. Even if you feel stable, your brain still needs the medication to stay balanced. Always work with your doctor to taper off slowly, if at all. Many people who quit on their own end up back in the hospital.
Why do I need blood tests for lithium if I feel okay?
Lithium’s safe range is very narrow. You can feel fine while your levels creep into the toxic zone. Symptoms like tremors, nausea, or confusion often appear only after damage has started. Blood tests catch this early. Skipping them is like driving with your eyes closed-you might not crash right away, but the risk is high.
Do antipsychotics make you gain weight no matter what?
Not all. Olanzapine and quetiapine are heavy weight gainers. But aripiprazole and lurasidone have minimal impact. If weight is a concern, ask your doctor about switching to one of these. Adding metformin can also help-many patients lose 5 to 10 pounds in six months. Lifestyle changes matter too: regular walking, cutting sugary drinks, eating protein-rich meals.
Is lamotrigine safe if I’m planning to get pregnant?
Lamotrigine is one of the safest mood stabilizers during pregnancy. Unlike valproate-which carries a 1-2% risk of neural tube defects-it has no known major birth defects. But you still need close monitoring. Your dose may need to be adjusted as your body changes during pregnancy. Always talk to your psychiatrist and OB-GYN before conceiving.
Can I use over-the-counter supplements with my bipolar meds?
Be very careful. Omega-3s and vitamin D are generally safe. But St. John’s Wort can trigger mania. Ginkgo biloba can interfere with lithium. Even high-dose vitamin B6 can affect how your body processes antipsychotics. Always tell your doctor about every supplement you take-even if you think it’s harmless.
How do I know if my medication isn’t working anymore?
Watch for early warning signs: sleeping less than 5 hours a night without feeling rested, sudden irritability, racing thoughts, or feeling unusually hopeless. If these last more than 3-4 days, contact your doctor. Medications can lose effectiveness over time, especially under stress. It’s not your fault. It’s biology. Adjustments are normal.
What Comes Next
If you’re on mood stabilizers or antipsychotics, your next step isn’t more pills. It’s better tracking. Start a simple mood journal: rate your energy, sleep, and mood on a scale of 1 to 10 each day. Note any new side effects. Bring it to every appointment.
Ask about genetic testing if you’ve tried three or more meds without success. Ask about long-acting injectables if you miss doses often. Ask about metformin if you’ve gained weight. Don’t wait until you’re in crisis.
Bipolar disorder is a lifelong condition. But with the right mix of science, self-awareness, and support, it doesn’t have to control your life. You just need to know what to look for-and when to speak up.

Taya Rtichsheva
December 9, 2025lithium made me drink so much water i started thinking i was a camel
also my hands shook like i was holding a phone during an earthquake
but hey at least i didnt try to jump off a bridge so i guess its a win
Tejas Bubane
December 10, 2025this is just a glorified drug pamphlet. nobody cares about your 2023 study metrics. real people don't live by blood test ranges and FDA approvals. they live by how much they can afford to pay for their meds and whether their insurance covers the metformin too
Richard Eite
December 11, 2025if you're taking antipsychotics and gaining weight you're just lazy
my cousin took quetiapine and ran marathons
you people need to get off the couch and stop blaming pills for your poor life choices
Olivia Portier
December 12, 2025i just want to say to anyone reading this: you're not broken
you're not failing if you need to switch meds
you're not weak for needing help
you're human
and you deserve to feel like yourself again
Brianna Black
December 13, 2025The pharmacological management of bipolar disorder represents a paradigmatic intersection of neurochemistry and existential resilience. One cannot understate the profound ontological weight carried by the lithium patient who endures tremors and thirst in service of temporal stability. This is not mere pharmacology-it is a metaphysical negotiation with the self.
Stacy Tolbert
December 15, 2025i took lamotrigine and got the rash
they said it was rare
but i looked in the mirror and thought i was turning into a tomato
and then i cried for three days
and then i stopped taking it
and then i felt like i was drowning
and then i started again
and now i'm just tired
Ronald Ezamaru
December 16, 2025you guys are forgetting the most important thing
the meds don't work if you don't sleep
if you don't eat
if you don't talk to someone
if you don't get sunlight
meds are just the base layer
the rest is survival
Ryan Brady
December 17, 2025lithium is for cowards who can't handle real meds
if you're on quetiapine and you're fat, that's your fault
and why are you even on reddit instead of working out?
Raja Herbal
December 19, 2025so you're telling me the same drug that saved your life also made you forget your daughter's birthday?
and you're okay with that?
huh. guess i'll just keep drinking chai and praying
Iris Carmen
December 19, 2025i started journaling after i forgot my own phone number for 2 days
now i write down my mood like its a weather report
today: cloudy with a 70% chance of crying
but at least i remember my name
Rich Paul
December 19, 2025cyp2d6 polymorphism is the real key here
you're not failing because you're weak
you're failing because your liver is genetically incompatible with the standard protocol
if you haven't done pharmacogenomics testing you're just guessing
and guessing is how people end up in psych wards
Delaine Kiara
December 21, 2025i tried lithium for 6 months
my hands shook so bad i couldn't hold a coffee cup
my weight went up 20 lbs
my doctor said 'it's working' but i felt like a ghost
so i quit
and then i got manic for 11 days
and then i went back on it
and now i'm just numb
but i'm alive
so i guess that's the win