13 Jan 2026
- 14 Comments
Goldenseal Medication Interaction Checker
Check for Goldenseal Interactions
Enter medications you're taking. Goldenseal can dangerously interact with many prescription drugs by inhibiting liver enzymes.
Interaction Results
Many people turn to goldenseal for colds, sinus infections, or digestive issues, believing it’s a natural way to boost immunity. But what they don’t realize is that this popular herb can quietly mess with medications they’re already taking-sometimes with serious consequences. If you’re on any prescription drugs, goldenseal isn’t just another supplement. It’s a potential time bomb for your liver’s ability to process medicine.
What Goldenseal Actually Does to Your Liver
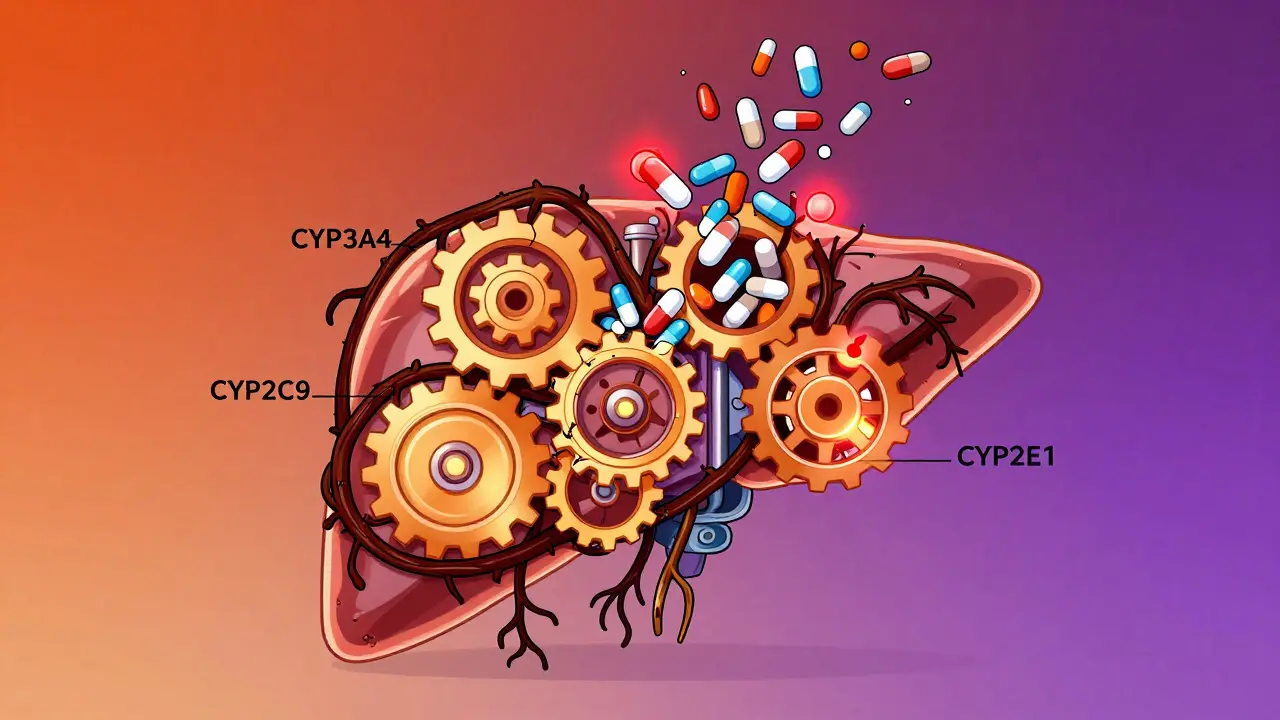
Goldenseal isn’t just a plant. It’s a chemical factory. Its main active ingredients-berberine and hydrastine-don’t just fight germs. They slam the brakes on your liver’s drug-processing system. Your liver uses a group of enzymes called cytochrome P450 (CYP) to break down about 75% of all prescription medications. Goldenseal blocks five of the most important ones: CYP3A4, CYP2D6, CYP2C9, CYP1A2, and CYP2E1.
That’s not a small thing. CYP3A4 alone handles half of all drugs you take-statins, blood pressure meds, anti-anxiety pills, even some cancer treatments. When goldenseal inhibits these enzymes, your body can’t clear medications the way it should. The result? Higher drug levels in your blood. Think of it like pouring gasoline into a car that’s already running full throttle. The engine doesn’t just go faster-it risks exploding.
Studies show goldenseal can boost the concentration of certain drugs by 40% to 60%. For someone on metoprolol for heart rhythm, that could mean dangerously low blood pressure. For someone on codeine, it could mean too much morphine builds up, leading to slowed breathing. And it doesn’t stop there. Goldenseal also blocks P-glycoprotein, a transporter that helps move drugs like digoxin and metformin in and out of cells. That’s why some users report wild swings in blood sugar or heart rate after taking goldenseal.
Which Medications Are Most at Risk?
Not all drugs are affected the same. But if you’re taking any of these, goldenseal is a hard no:
- Statins (simvastatin, atorvastatin): Risk of muscle damage or liver toxicity
- Blood pressure meds (lisinopril, metoprolol): Can cause dizziness, fainting, or dangerously low BP
- Anticoagulants (warfarin): Goldenseal can spike INR levels by 1.5 to 2.0 points-putting you at risk of bleeding
- Immunosuppressants (cyclosporine, tacrolimus): Levels can rise 30-50%, increasing risk of kidney damage or infection
- Diabetes drugs (metformin): Goldenseal can either raise or lower blood sugar unpredictably
- Antidepressants (fluoxetine, sertraline): Higher levels can lead to serotonin syndrome
- Benzodiazepines (midazolam, triazolam): Increased sedation, confusion, or respiratory depression
A 2018 clinical trial found that just one dose of goldenseal increased fluoxetine levels by 55%. Another case in 2022 showed a diabetic patient’s HbA1c jumped from 6.8% to 8.2% in four weeks after adding goldenseal to their routine. That’s not a coincidence. That’s a direct interaction.
Why Goldenseal Is More Dangerous Than Other Herbs
You’ve probably heard about grapefruit juice or St. John’s wort messing with meds. Goldenseal is worse. Grapefruit juice mainly hits CYP3A4. St. John’s wort induces enzymes, making drugs less effective. Goldenseal does something far more unpredictable-it inhibits multiple enzymes at once.
According to a 2020 review in Drug Metabolism Reviews, goldenseal ranks third among 15 common herbal supplements for interaction risk-behind only grapefruit juice and St. John’s wort. But unlike St. John’s wort, which you can time around your meds, goldenseal’s effects linger. It doesn’t just stop working the day you quit. Studies show its inhibition of liver enzymes can last 7 to 14 days after your last dose.
And here’s the kicker: supplements aren’t regulated like drugs. A 2022 USP study found only 38% of goldenseal products had berberine levels within 20% of what was on the label. One bottle might have 0.5% berberine. The next might have 8%. You can’t predict how much you’re actually taking. That’s why two people taking the same dose can have wildly different reactions.

Real Stories: What Happens When People Ignore the Warnings
Reddit threads and patient reviews tell the real story. One user, 'HypertensionWarrior,' reported fainting and a blood pressure reading of 85/50 after combining goldenseal with lisinopril. They ended up in the ER. Another user on MedicineNet said their blood sugar went haywire after adding goldenseal to their metformin regimen. No one warned them.
These aren’t rare. The FDA received 59 goldenseal-related adverse event reports in 2022-up from 43 in 2018. Most involved people who didn’t tell their doctor they were taking it. Why? Because they thought it was “natural,” so it must be safe. But natural doesn’t mean harmless. Willow bark contains salicin-like aspirin. Foxglove contains digitalis-like heart medication. Nature doesn’t care about your intentions. It only cares about chemistry.
What Should You Do If You’re Already Taking Goldenseal?
If you’re currently using goldenseal and taking any prescription meds, don’t just quit cold turkey. Talk to your pharmacist or doctor. But here’s what you need to know right now:
- Stop goldenseal immediately if you’re on any of the high-risk medications listed above.
- Wait two weeks after your last dose before starting or adjusting any medication metabolized by CYP enzymes. The effects don’t vanish overnight.
- Check your meds. Use the American Society of Health-System Pharmacists’ free CYP interaction checker. It lists 147 medications with known or potential interactions with goldenseal.
- Don’t assume “natural” means safe. If a supplement doesn’t have a FDA-approved drug label, it’s not tested for safety with other medicines.
Some people swear by goldenseal for short-term sinus relief. But even those cases show a pattern: the positive reviews (62% of them) say they only used it when not on any prescription meds. That’s not a coincidence. That’s the only safe scenario.

The Bigger Picture: Why This Keeps Happening
The supplement industry made $18.7 million selling goldenseal in 2022. But only 3% of U.S. adults use it regularly. Most are older adults-ages 45 to 64-who are also the most likely to be on multiple medications. They’re the ones at highest risk.
Meanwhile, the FDA has warned 12 companies for making illegal claims that goldenseal treats infections. The European Medicines Agency outright banned it for medicinal use. Yet here in the U.S., it’s still on shelves, marketed as a “natural immune booster.”
The NIH is now funding a $2.3 million clinical trial to study goldenseal’s interactions with 10 common drugs. Results won’t be out until late 2025. But we already know enough to say: if you’re on meds, don’t risk it.
There’s no evidence goldenseal cures colds. There’s plenty of evidence it can hurt you.
What’s the Alternative?
If you want to support your immune system without risking dangerous interactions, stick with what’s proven: sleep, hydration, vitamin D, and zinc. If you have a persistent infection, see a doctor. Don’t reach for a bottle that could be silently poisoning your medication’s effectiveness.
Goldenseal isn’t the villain. It’s a tool with no safety label. And tools without labels are dangerous in the hands of people who don’t know how they work.
Can I take goldenseal if I’m not on any medications?
Even if you’re not on medications now, it’s still risky. Goldenseal can affect liver enzymes for up to two weeks after you stop taking it. If you later start a new prescription-like a statin, blood pressure drug, or antidepressant-you could still have an interaction. It’s safer to avoid it entirely unless you’re under direct medical supervision.
How long does goldenseal stay in your system?
The active compounds in goldenseal, especially berberine, can inhibit liver enzymes for 7 to 14 days after your last dose. This means even if you stop taking it a week before starting a new medication, you’re not necessarily safe. A two-week washout period is the standard recommendation from pharmacists.
Is there a safe dose of goldenseal?
There’s no proven safe dose when combined with medications. Even low doses can inhibit liver enzymes. Plus, supplement labels are unreliable-berberine levels vary from 0.5% to 8% across brands. You can’t trust the dose, so you can’t trust the safety.
Can I take goldenseal with over-the-counter painkillers?
Be careful. Goldenseal inhibits CYP2E1, which metabolizes acetaminophen (Tylenol). This can lead to higher levels of acetaminophen in your blood, increasing the risk of liver damage-even at normal doses. Avoid combining them. Use ibuprofen or naproxen instead, but still check with your pharmacist.
Why do some people say goldenseal works for them?
Some people report benefits because they’re not on medications that interact with it. Or they used it for just a few days during a minor cold. But those are anecdotal, not scientific. There’s no strong evidence goldenseal treats infections better than rest, fluids, or time. The risks far outweigh any unproven benefits.

vishnu priyanka
January 14, 2026Man, I’ve seen this in India too-people buy goldenseal from Amazon, mix it with their blood pressure pills, and wonder why they’re dizzy. Nature doesn’t care if you call it ‘herbal.’ It’s chemistry, baby.
Alan Lin
January 16, 2026This is one of the most important posts I’ve read all year. I’m a pharmacist, and I see this exact scenario every single week. Patients say, ‘But it’s natural!’ Like that means it doesn’t interact with warfarin or metformin. The disconnect is terrifying. Please share this with everyone you know.
Clay .Haeber
January 18, 2026Oh wow, so goldenseal’s not just some hippie tea-it’s a liver-slamming, enzyme-crippling, FDA-waiting-to-happen disaster? Who knew? I guess ‘natural’ is just the supplement industry’s way of saying ‘I didn’t run any clinical trials, but my cousin swears by it.’
Gregory Parschauer
January 19, 2026You people are so naive. You think just because something comes from a plant, it’s harmless? That’s like saying a rattlesnake is harmless because it’s ‘organic.’ Goldenseal is a potent pharmacological agent disguised as wellness. It’s not ‘natural’-it’s pharmaceutical-grade interference with zero labeling. If you’re on meds and you’re still taking this, you’re not just ignorant-you’re endangering lives. Including your own.
Pankaj Singh
January 19, 2026Let me guess-next you’ll tell us turmeric doesn’t thin blood or ginger doesn’t lower BP. This is why America’s dying. Everyone’s too lazy to read the damn label or talk to a doctor. You want ‘natural’? Go eat garlic and sleep 8 hours. Stop swallowing bottles labeled ‘immune booster’ like they’re candy.
Nelly Oruko
January 20, 2026the fact that 38% of goldenseal products have berberine levels within 20% of what's on the label... that's not a flaw. that's a crime. how can we trust anything in this industry when the math doesn't even add up? i'm not even mad. i'm just... disappointed.
Diana Campos Ortiz
January 21, 2026I took goldenseal for three days during a bad cold last year-no meds, just pure curiosity. I felt fine. But after reading this? I threw the rest out. Better safe than sorry. Thanks for the clarity.
Jesse Ibarra
January 22, 2026Oh, so now we’re policing what people put in their bodies? Next they’ll ban kale because it’s ‘too potent’ and ‘interacts with thyroid meds.’ This is the slippery slope of medical authoritarianism disguised as ‘education.’ You think people are stupid? Maybe you’re just not explaining it right.
Angel Molano
January 23, 2026If you’re on meds and take goldenseal, you deserve what happens. No one’s forcing you to be reckless.
Robin Williams
January 25, 2026stop being scared of nature. we’ve been medicating ourselves to death since the 1950s. maybe the answer isn’t more pills but less interference. goldenseal has been used for centuries. maybe the problem isn’t the herb-it’s our broken system.
Vinaypriy Wane
January 27, 2026I understand the science. I really do. But I also know people who’ve used goldenseal for years-no issues. Maybe it’s about dosage. Maybe it’s about quality. Maybe it’s about context. I’m not saying it’s safe. I’m saying it’s not black and white. And we owe it to people to talk about nuance, not fear.
Randall Little
January 28, 2026So if I take goldenseal on Tuesday and start a new statin on Friday, I’m still at risk? Even if I didn’t take it for 3 days? That’s wild. So the inhibition lingers like a ghost in the liver? That’s… honestly terrifying. I’m deleting my goldenseal stash right now.
Adam Vella
January 28, 2026It is a well-documented phenomenon in pharmacokinetics that phytochemicals-particularly alkaloids such as berberine-exert potent inhibitory effects upon the cytochrome P450 isoenzyme family, specifically CYP3A4 and CYP2D6, thereby altering the metabolic clearance of co-administered pharmaceutical agents. This is not speculative; it is empirically validated through in vitro, in vivo, and clinical studies. The regulatory vacuum surrounding dietary supplements permits the commercialization of products with inconsistent bioactive concentrations, thereby introducing unpredictable pharmacodynamic outcomes. Consequently, the assertion that goldenseal poses a clinically significant risk is not only substantiated but is, in fact, an understatement.
Kimberly Mitchell
January 29, 2026Why are we even talking about this? Nobody reads labels anyway. Just let people die if they want to.