1 Feb 2026
- 13 Comments
G6PD Deficiency Risk Assessment Tool
This tool helps you understand your risk of having G6PD deficiency, which can lead to serious hemolytic anemia when taking the common antibiotic nitrofurantoin.
What is this tool for?
G6PD deficiency is a genetic condition that makes some people vulnerable to hemolytic anemia when taking certain medications like nitrofurantoin. This tool assesses your risk based on your ancestry and medical history. If you're at higher risk, we recommend getting tested.
Every year, millions of people take nitrofurantoin to treat a simple urinary tract infection. It works fast, it’s cheap, and for most people, it’s safe. But for a significant number of others, this common antibiotic can trigger a life-threatening reaction they never knew they were at risk for: hemolytic anemia caused by an undiagnosed genetic condition called G6PD deficiency.
What Is Nitrofurantoin, and Why Is It So Common?
Nitrofurantoin, sold under brand names like Macrobid and Furadantin, has been around since the 1940s. It’s not a flashy drug. It doesn’t cure pneumonia or sepsis. But for uncomplicated bladder infections - the kind that make you pee constantly and burn when you go - it’s one of the most effective options. Unlike many antibiotics, bacteria haven’t developed strong resistance to it. About 10-15% of E. coli strains are resistant, compared to 20-25% for trimethoprim-sulfamethoxazole, another go-to UTI drug.
It’s also targeted. Nitrofurantoin doesn’t flood your whole body. It concentrates in your urine, where it kills the bacteria causing the infection. That’s why it’s often the first choice for doctors treating healthy adults with no kidney problems. In the U.S. alone, about 5.5 million prescriptions are filled each year.
What Is G6PD Deficiency - And Why Does It Matter?
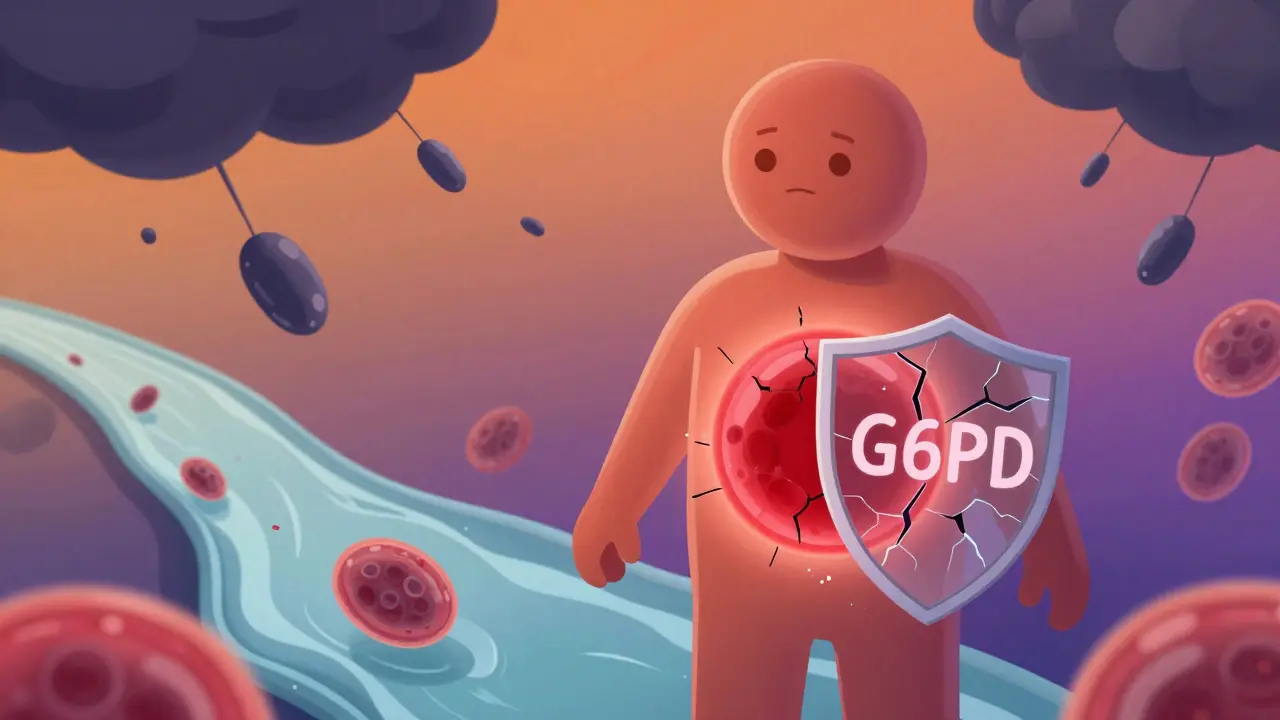
Glucose-6-phosphate dehydrogenase (G6PD) is an enzyme your red blood cells need to protect themselves from oxidative stress. Think of it like a shield. When your body breaks down toxins, produces energy, or fights infection, it creates reactive molecules called free radicals. G6PD helps neutralize them so your red blood cells don’t get damaged.
But if you’re born with G6PD deficiency - and about 400 million people worldwide are - that shield is weak or missing. You might never know it… until something like nitrofurantoin comes along.
Nitrofurantoin doesn’t just kill bacteria. In your body, it turns into reactive, oxidizing compounds. In people with normal G6PD, those compounds are handled easily. In someone with G6PD deficiency, the red blood cells can’t defend themselves. The hemoglobin inside them starts to clump and break down. The cells burst. That’s hemolysis. And when enough red blood cells are destroyed at once, you get acute hemolytic anemia.
How Dangerous Is This Reaction?
It’s not rare. A 2022 review of medical literature found 42 confirmed or highly probable cases of nitrofurantoin-induced hemolytic anemia in G6PD-deficient patients. Ten of those cases ended in death. Most happened within 24 to 72 hours of starting the drug.
Symptoms come on fast: sudden fever, chills, dark urine (like cola), extreme fatigue, yellowing skin or eyes, rapid heartbeat, and dizziness. In severe cases, people collapse from low blood pressure. One case report described a patient whose hemoglobin dropped from 14 g/dL to 7.2 g/dL in under 72 hours - a drop that would send most people straight to the ER.
What’s scary is how quickly it can be missed. Many doctors don’t think to ask about ancestry or family history. They just see a UTI and reach for the most common, cheapest antibiotic. And here’s the problem: if you’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent, your chance of having G6PD deficiency is much higher - up to 14% in some groups. Yet screening isn’t routine.

Who’s Most at Risk?
It’s not just adults. Infants exposed to nitrofurantoin through breast milk have developed hemolytic anemia. Pregnant women with undiagnosed G6PD deficiency who took the drug also had serious reactions. In fact, eight documented cases involved pregnant patients.
And here’s the twist: even if you’ve taken nitrofurantoin before without issues, that doesn’t mean you’re safe. G6PD deficiency can be mild. You might only react under stress - like an infection, certain foods (fava beans), or a new drug. A person could take nitrofurantoin safely at 25, then have a crisis at 45 after a viral illness weakens their system further.
What Do Experts Say About Screening?
The American Society of Hematology, the Clinical Pharmacogenetics Implementation Consortium (CPIC), and the European Medicines Agency all agree: avoid nitrofurantoin in patients with known G6PD deficiency.
But here’s the gap: the FDA label only says, “Hemolytic anemia has been reported in G6PD-deficient individuals.” It doesn’t require testing. No mandatory screen. No checklist. No alert in most electronic health records.
A 2022 survey of 350 primary care doctors found only 32% routinely check for G6PD deficiency before prescribing nitrofurantoin. That means nearly 7 out of 10 patients are being put at risk without anyone asking.
Meanwhile, G6PD testing costs $35-$50. A hospital stay for hemolytic anemia? That averages $8,500-$12,000. You’re spending less to prevent a crisis than you’d pay to treat one.
What Are the Alternatives?
If you have G6PD deficiency - or you’re from a high-risk population - there are safer options.
- Fosfomycin: A single-dose antibiotic, often used as first-line for UTIs in G6PD-deficient patients. It’s not affected by the same oxidative pathways.
- Pivmecillinam: Available in many countries, not yet approved in the U.S., but widely used in Europe with low hemolytic risk.
- Cephalexin: A first-generation cephalosporin. While some cephalosporins can cause immune-mediated hemolysis, this one doesn’t trigger oxidative damage.
- Trimethoprim-sulfamethoxazole: Higher resistance rates, but generally safe for G6PD-deficient patients - unless they have a history of sulfa allergy.
For patients with kidney problems, options shrink. Nitrofurantoin is already off the table if your eGFR is below 60. But so are many other drugs. That’s why knowing your G6PD status matters even more - it helps doctors pick the right drug without guessing.
What Should You Do?
If you’ve ever been told you have anemia, jaundice as a baby, or a family history of blood disorders - especially if you’re of African, Mediterranean, Middle Eastern, or Southeast Asian descent - ask your doctor for a simple G6PD blood test. It’s a quick finger-prick or venous draw. Results come back in hours.
If you’re prescribed nitrofurantoin and you don’t know your status, ask: “Is this safe for someone with G6PD deficiency?” Don’t be afraid to push back. Your life might depend on it.
If you’ve already taken nitrofurantoin and developed symptoms like dark urine, fatigue, or yellowing skin within a few days - stop the drug immediately and get medical help. Hemolytic anemia from nitrofurantoin is treatable if caught early. Most patients recover fully within 48 hours after stopping the drug and getting fluids.
The Bigger Picture
Nitrofurantoin isn’t going away. It’s too effective against resistant UTIs. But the medical world is slowly waking up. Point-of-care G6PD tests are being developed - imagine a test you can do in the doctor’s office while you wait. The NIH is running a trial to see if universal screening before prescribing nitrofurantoin saves money and lives. Early results are promising.
Right now, we’re treating UTIs like they’re all the same. But they’re not. One size doesn’t fit all - especially when genetics play a role. The future of antibiotics isn’t just about resistance. It’s about matching the right drug to the right person.
Don’t wait for a crisis to find out you’re at risk. Ask. Test. Know. It’s simple. And it could save your life.
Can nitrofurantoin cause hemolytic anemia in people without G6PD deficiency?
Rarely. Most cases of nitrofurantoin-induced hemolytic anemia occur in people with G6PD deficiency. While other immune-mediated reactions can happen, they’re extremely uncommon. The vast majority of serious hemolytic events are linked to the oxidative stress caused by nitrofurantoin in G6PD-deficient individuals.
Is G6PD deficiency only a problem in certain ethnic groups?
No, but prevalence varies. It’s most common in people of African descent (10-14%), Mediterranean and Middle Eastern descent (4-7%), and Southeast Asian descent (2-5%). It’s less common in Northern Europeans and East Asians, but still possible. If you have ancestry from any of those regions, you should consider testing - even if you’ve never had symptoms.
Can I take nitrofurantoin if I have G6PD deficiency but never had a reaction before?
No. G6PD deficiency is a lifelong condition. Just because you took nitrofurantoin before without issues doesn’t mean you’re safe. Your body’s ability to handle oxidative stress can change with age, illness, or other medications. The risk remains. Experts recommend complete avoidance.
Does G6PD testing hurt or take long?
No. It’s a simple blood test - often just a finger prick. Results can be ready in under an hour with point-of-care tests, or within a day in a lab. The test doesn’t require fasting or special preparation. It’s quick, painless, and far less risky than the reaction it prevents.
What if I’m pregnant and need a UTI antibiotic?
Nitrofurantoin is generally avoided in late pregnancy due to potential neonatal effects, and especially in women with unknown G6PD status. Fosfomycin and cephalexin are preferred. If you’re from a high-risk ethnic group, ask your OB-GYN to check your G6PD status before any UTI treatment. A single dose of fosfomycin is often enough and is considered safe during pregnancy.
Can children be tested for G6PD deficiency?
Yes. Newborn screening for G6PD deficiency is routine in some countries and recommended for infants with unexplained jaundice or a family history. If your child has had a reaction to sulfa drugs, fava beans, or naphthalene (mothballs), testing is strongly advised. It’s safe and critical before giving any oxidizing antibiotics like nitrofurantoin.

Solomon Ahonsi
February 1, 2026This is such a bullshit oversight. Doctors prescribe this like it's water and then act shocked when someone drops dead from it. No one asks about your ancestry. No one checks. It's cheaper to kill people than to run a $50 test. Welcome to American healthcare.
George Firican
February 2, 2026The tragedy here isn't just the lack of screening-it's the systemic blindness to genetic variance in medicine. We treat human bodies like they're mass-produced widgets, when in reality, our biology is as diverse as our languages. Nitrofurantoin isn't the villain; it's the symptom of a system that refuses to see individuality. We've got the tools. We've got the data. What we lack is the will to use them.
Matt W
February 4, 2026I had a cousin who got hospitalized after taking this for a UTI. They didn't even know she was G6PD deficient until she turned yellow and couldn't walk. She's fine now, but it took three days and a blood transfusion. Please, if you're from anywhere near Africa, the Med, or South Asia-just get tested. It's one prick. It could save you.
Anthony Massirman
February 5, 2026Just get tested. Seriously. Five minutes. Done.
Ansley Mayson
February 6, 2026Why are we even talking about this? If you're from one of those countries you should just avoid antibiotics altogether. Stop making everything a race issue.
phara don
February 8, 2026Wait so if I'm mixed race-like half Nigerian, half Irish-do I still need the test? Or is it like a sliding scale of risk?
Murarikar Satishwar
February 10, 2026As someone from India, I never knew this was a thing. My uncle took this for a UTI in 2018 and ended up in ICU. We thought it was just food poisoning. This post is eye-opening. Doctors here don't even mention G6PD. I'm getting tested tomorrow. Thank you for sharing.
Bob Hynes
February 11, 2026Man I just got prescribed this last week… and I’m half Lebanese. I’m gonna call my doc right now and be like hey can we do the thing with the finger poke? I don’t wanna end up looking like a banana from the inside.
Eli Kiseop
February 11, 2026so if you take it once and nothing happens you're fine right
Sandeep Kumar
February 13, 2026Western medicine is so lazy. In India we test for this before giving any drug. But here you wait till someone dies then write a blog. Pathetic.
Gary Mitts
February 15, 2026Yeah because nothing says "I care about your health" like a $50 test instead of a $10k ER bill. Thanks capitalism.
clarissa sulio
February 15, 2026I'm so glad this is getting attention. My sister had this happen and no one connected the dots. We need mandatory screening. It's not hard.
Bridget Molokomme
February 16, 2026Wow so you're saying we should test everyone before giving them antibiotics? Next you'll tell us to check for allergies before giving them water.