16 Dec 2025
- 12 Comments
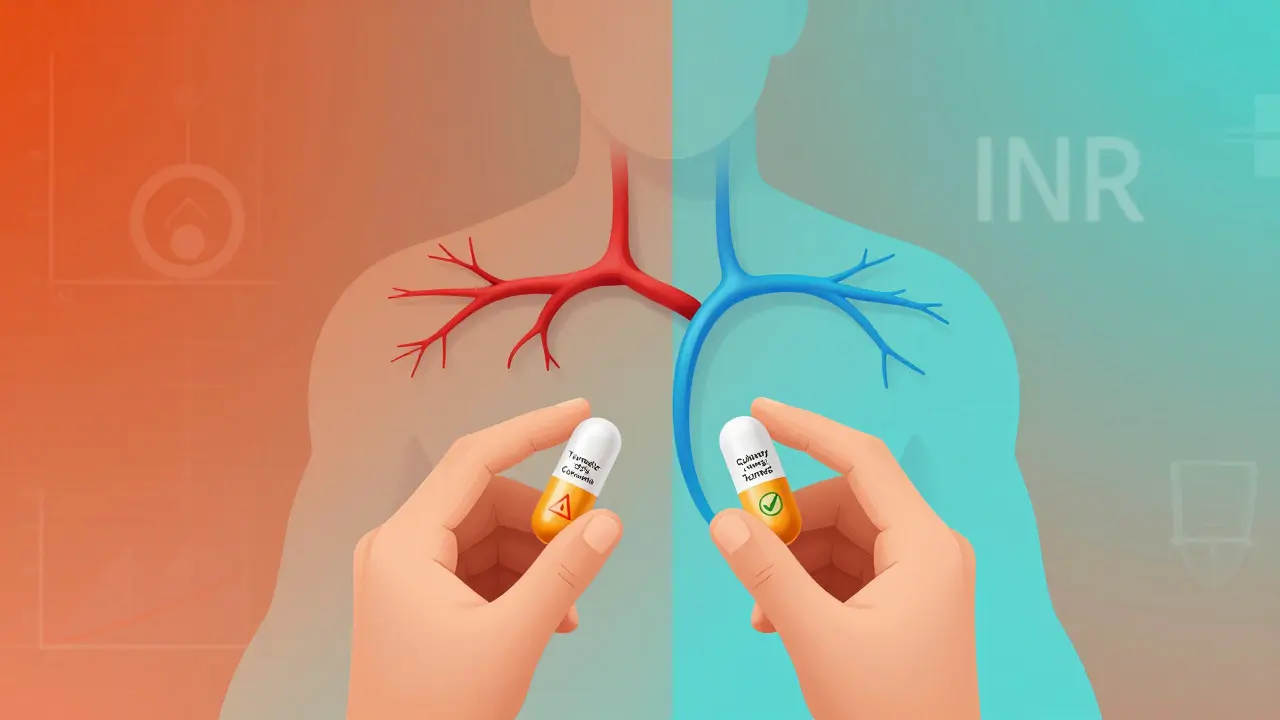
Millions of people take turmeric daily-sprinkled on eggs, blended into smoothies, or swallowed in capsules-because it’s "natural," "anti-inflammatory," and "good for you." But if you’re on a blood thinner like warfarin, clopidogrel, or rivaroxaban, that daily spoonful could be dangerous. The science isn’t murky. It’s clear: turmeric and curcumin can dangerously amplify the effects of blood thinners, pushing your INR into life-threatening territory.
How Turmeric Acts Like a Blood Thinner
Turmeric isn’t just a spice. Its main active ingredient, curcumin, directly interferes with how your blood clots. Unlike prescription anticoagulants that target one specific pathway, curcumin hits multiple targets at once. It slows down thrombin and factor Xa-two key proteins your body uses to form clots. It also reduces platelet aggregation, meaning your blood cells stick together less easily. This dual action makes it a potent natural anticoagulant.A 2012 study published in PubMed found that curcumin prolonged both aPTT and PT-standard lab tests that measure how long it takes your blood to clot. The higher the dose, the stronger the effect. Even more concerning: curcumin’s anticoagulant effect was actually stronger than its derivative, bisdemethoxycurcumin. That means the very compound that gives turmeric its bright yellow color is also the one most responsible for the risk.
Compare that to warfarin, which blocks vitamin K recycling, or DOACs like Eliquis or Xarelto, which block factor Xa directly. Those drugs are dosed precisely, monitored with blood tests, and studied in tens of thousands of patients. Turmeric? One capsule might have 2% curcumin. Another might have 95%. There’s no standard. No safety label. Just guesswork.
Real Cases, Real Danger
This isn’t theoretical. It’s happened.In 2018, Medsafe in New Zealand reported a case where a patient on stable warfarin therapy had an INR of 10.3 after starting a turmeric supplement. The therapeutic range for warfarin is 2 to 3.5. An INR above 5 is already considered high risk. Above 9? That’s emergency territory. This patient didn’t have a fall or injury. They just added a supplement they thought was harmless. The result? A near-fatal bleeding risk.
Another case, documented by the Welsh Medicines Information Centre, involved a transplant patient taking tacrolimus-a drug that prevents organ rejection. After consuming 15 or more spoonfuls of turmeric powder daily for ten days, their tacrolimus levels spiked to 29 ng/mL (normal range: 5-15). That’s toxic. They developed acute kidney injury. Turmeric wasn’t just thinning their blood-it was interfering with how their liver processed other critical medications.
These aren’t outliers. They’re red flags. And they’re not rare. The WMIC confirmed in October 2024 that curcumin can reduce the clearance of warfarin from the body, meaning it lingers longer, increasing its effect. When you’re already on a drug with a narrow therapeutic window, even a small increase in concentration can tip you into bleeding.
Which Blood Thinners Are Riskiest?
All of them. But some are riskier than others.Warfarin (Coumadin) is the most dangerous combo. Why? Because it has a very narrow range between effective and toxic. A tiny change in how your body processes it can send your INR soaring. Curcumin doesn’t just add to warfarin’s effect-it changes how your liver metabolizes it, making the drug stick around longer. That’s why the WMIC and Medsafe both specifically warn about warfarin.
DOACs like rivaroxaban (Xarelto), apixaban (Eliquis), and dabigatran (Pradaxa) are often seen as "safer" because they don’t require regular INR checks. But that doesn’t mean they’re safe with turmeric. The British Heart Foundation explicitly warns that high-dose turmeric supplements can interact with these drugs too. Curcumin inhibits the same enzymes (CYP3A4 and P-glycoprotein) that help clear DOACs from your body. That means more drug, more bleeding risk.
Antiplatelets like aspirin, clopidogrel (Plavix), and even over-the-counter NSAIDs like ibuprofen or naproxen also raise the risk. Turmeric doesn’t just thin blood-it prevents platelets from clumping. Combine that with aspirin, which does the same thing, and you’re doubling down on bleeding risk. There’s no buffer. No safety net.
How Much Turmeric Is Dangerous?
You might think, "I just use it in cooking. I’m fine." And you probably are.Regular culinary use-half a teaspoon in curry or soup-is unlikely to cause issues. The amount of curcumin you get from food is low, and your body doesn’t absorb it well without black pepper or fat. But supplements? That’s a different story.
Most turmeric supplements contain 500-1,000 mg of curcumin per capsule. That’s the equivalent of eating 25-50 grams of raw turmeric root daily. That’s not cooking. That’s pharmaceutical dosing. And no supplement label tells you that.
Even "standardized" extracts vary wildly. One brand might have 95% curcumin. Another might have 5%. There’s no FDA oversight. No batch testing. You’re taking a gamble every time you open that bottle.
What Doctors Say
The medical consensus is blunt.Medsafe says: "Concurrent use... should be avoided." Mayo Clinic says: "Turmeric in large doses can act like a blood thinner, causing bleeding or dangerously enhancing the effects of blood-thinning medications." The Welsh Medicines Information Centre says: "Monitor closely if warfarin and curcumin are taken together... especially as warfarin has a narrow therapeutic index." And Dr. Oracle’s 2023 analysis says it plainly: "The evidence clearly indicates that the anticoagulant properties of turmeric/curcumin create a significant risk when combined with warfarin." These aren’t opinions. They’re warnings based on documented cases, lab studies, and pharmacokinetic data. The British Heart Foundation now includes turmeric in its official guidance on drug interactions. That’s not a footnote. That’s policy.

What You Should Do
If you’re on any blood thinner:- Stop taking turmeric supplements immediately. No "maybe," no "I’ll cut back." Stop.
- Don’t assume "natural" means safe. Aspirin was once considered natural too. So was digitalis. Both can kill.
- Talk to your doctor or pharmacist. Bring your supplement bottle. Show them the label. Ask: "Could this interfere with my medication?"
- Stop turmeric supplements at least two weeks before any surgery or dental procedure. Even minor ones. Bleeding during a tooth extraction can be serious if your blood won’t clot.
- Don’t replace your prescription with turmeric. There’s no evidence it’s as effective as warfarin or DOACs for preventing strokes or clots.
If you love turmeric for flavor, keep using it in cooking. But don’t confuse flavor with medicine. A pinch in your rice won’t hurt. A capsule labeled "1,000 mg curcumin" might.
The Bigger Problem
The real danger isn’t just the interaction. It’s the gap between what people believe and what science says.Most people think supplements are harmless because they’re "natural." They don’t realize that "natural" doesn’t mean "safe." It doesn’t mean "tested." It doesn’t mean "regulated."
Meanwhile, 2-3% of adults in the U.S. and Europe are on blood thinners. That’s millions of people. And many of them are taking turmeric supplements without knowing the risk. They’re reading blogs that say "turmeric prevents blood clots"-and missing the part that says "so does your medication."
This isn’t about fear. It’s about facts. The data is solid. The cases are real. The consequences-internal bleeding, stroke, death-are irreversible.
If you’re on a blood thinner, treat turmeric supplements like you would a new prescription: with caution, with questions, and with your doctor’s approval.
Can I still use turmeric as a spice in cooking if I’m on blood thinners?
Yes, using turmeric as a spice in food is generally safe. The amount of curcumin you get from cooking-like a half-teaspoon in curry or soup-is too low to significantly affect blood clotting. The real risk comes from concentrated supplements, not culinary use. But if you’re eating large amounts daily (more than a tablespoon), even in food, talk to your doctor.
How long does it take for turmeric to affect blood thinners?
It can happen quickly. In the documented case reported by Medsafe, a patient’s INR jumped from stable to over 10 within weeks of starting turmeric supplements. Some people may see changes in their INR within days, especially if they’re taking high-dose capsules or have a sensitive metabolism. There’s no universal timeline, but don’t wait for symptoms-get tested if you start a supplement.
Is there a safe dose of curcumin if I’m on warfarin?
There is no established safe dose. Studies haven’t defined a threshold where curcumin stops interacting with warfarin. Because warfarin has a narrow therapeutic range and curcumin supplements vary wildly in potency, even small amounts could be risky. Medical authorities recommend avoiding curcumin supplements entirely if you’re on warfarin or other blood thinners.
What are the signs that turmeric is interacting with my blood thinner?
Watch for unexplained bruising, nosebleeds, bleeding gums, blood in urine or stool, unusually heavy periods, or prolonged bleeding from cuts. More serious signs include severe headaches, dizziness, weakness, or sudden pain/swelling in limbs-these could signal internal bleeding. If you notice any of these after starting turmeric, stop the supplement and get medical help immediately.
Should I tell my surgeon if I take turmeric supplements?
Yes, absolutely. Surgeons and anesthesiologists need to know about every supplement you take, including turmeric. Even if you’ve been taking it for years, stopping it two weeks before surgery reduces bleeding risk. Many patients don’t mention supplements because they don’t think they matter. But they do. This isn’t optional information-it’s critical for your safety.
Are there any safe alternatives to turmeric for inflammation?
Yes. Fish oil (omega-3s) has mild anti-inflammatory effects and is generally safe with blood thinners at standard doses (under 3 grams per day). Ginger may also help, but like turmeric, it has mild anticoagulant properties-use cautiously. For reliable, evidence-based inflammation control, talk to your doctor about prescription options like low-dose NSAIDs (if appropriate) or physical therapies. Never replace prescribed treatment with unproven supplements.

amanda s
December 18, 2025This is why America is falling apart-people take supplements like they’re candy and then wonder why they’re bleeding out. No one checks with a doctor anymore. Just pop a pill labeled 'natural' and call it health. Wake up. This isn’t a yoga retreat, it’s your bloodstream.
Jigar shah
December 18, 2025The science here is robust and well-documented. Curcumin inhibits CYP3A4 and P-gp, both critical for metabolizing warfarin and DOACs. The 2012 study cited shows dose-dependent prolongation of PT and aPTT. Culinary use is negligible, but supplements bypass bioavailability barriers. This isn't alarmism-it's pharmacokinetics.
Jonathan Morris
December 19, 2025Let’s be real-Big Pharma hates this. Turmeric is cheaper than warfarin. They’ve been suppressing studies for decades. Why do you think the FDA doesn’t regulate supplements? Because they’re owned by the same corporations that sell blood thinners. This is a profit-driven cover-up. That Medsafe case? Probably silenced. Look at the funding behind the 'official' warnings.
Linda Caldwell
December 21, 2025Y’all need to stop panicking and start listening to your body. If you’re on blood thinners and feel weird after turmeric-stop. But don’t blame the spice. Blame the lack of education. We’re taught to fear chemicals, not to question 'natural' labels. Simple fix: talk to your pharmacist. They’re the real heroes.
CAROL MUTISO
December 23, 2025It’s hilarious how we’ve turned wellness into a cult where the only sin is not buying the right powder. Turmeric isn’t evil-it’s just been weaponized by marketers who know we’ll swallow anything if it glows yellow. The real tragedy? People think they’re being 'proactive' about health while ignoring the only thing that matters: evidence. And yet, here we are, arguing about spices instead of demanding regulation.
Virginia Seitz
December 24, 2025Spice good. Capsules bad. 🙃
Brooks Beveridge
December 26, 2025Hey, if you’re on blood thinners and you’re reading this-you’re already ahead of most people. Seriously. Most folks don’t even know what INR means. Take this seriously, but don’t freak out. Talk to your doc. Bring your bottle. They’ve seen it all. And if you love turmeric? Keep using it in your dal. That’s where it belongs.
Kent Peterson
December 28, 2025Wait-so now we’re banning turmeric? Next they’ll ban garlic, ginger, and cinnamon. Who’s next? The FDA? The WHO? The Wellness Police? This is socialism disguised as medicine. If I want to eat a pound of turmeric and bleed out, that’s my right. You want to control my spice cabinet? Try harder.
Josh Potter
December 29, 2025bro i took turmeric capsules for 3 months while on Xarelto and i’m still alive lmao. maybe it’s just me? maybe the docs are just scared of free stuff? i’m not gonna stop. i’m 28, i’m healthy, and i don’t trust big pharma. #turmericlife
Evelyn Vélez Mejía
December 30, 2025One cannot overstate the epistemological rupture between folk medicine and evidence-based pharmacology. The conflation of culinary tradition with pharmacological intervention constitutes a dangerous ontological category error. Curcumin’s inhibition of coagulation factors is not a 'natural benefit,' but a quantifiable, dose-dependent biochemical interaction that demands clinical vigilance. To dismiss this as 'hype' is to abdicate the responsibility of informed agency.
Victoria Rogers
December 31, 2025lol who even uses turmeric anymore? i mean, like, it’s so 2018. everyone’s doing ashwagandha now. also i think this whole thing is overblown. my grandma ate turmeric paste every day and lived to 97. maybe the real problem is that people are too weak to handle their own bodies?
Nishant Desae
January 2, 2026I come from a family in India where turmeric is part of every meal, every ritual, every remedy. My father took it daily for arthritis. He was on warfarin for atrial fibrillation. We didn’t know about the interaction until he had a minor bleed after a fall. We thought it was just old age. This post saved my uncle’s life-he stopped supplements after reading this. So thank you. But also, please remember: culture and science aren’t enemies. We can honor tradition and still learn. Maybe the answer isn’t to ban turmeric-but to teach people how to use it wisely, with awareness, not fear.